Introduction
Plantar fasciitis is a condition characterized by sharp pain localized at the heel that is often due to repetitive strain or overuse causing microtears to the plantar fascia’s origin on the medial calcaneal tuberosity and often multifactorial in etiology (Rhim et al. 2021). This condition leads to an estimated 1 million patient visits per year (Nahin 2018). Non-operative interventions such as rest, plantar fascia specific stretches, anti-inflammatory medications, corticosteroid injections, orthotics, and night splints are often used in combination as first-line treatments. Approximately,10% of these patients develop chronic heel pain (Davis, Severud, and Baxter 1994). If non-operative treatments fail, a patient may proceed with an endoscopic or open plantar fascia release. Endoscopic approach shows shorter recovery times (Chou, Ng, and Koo 2016) and fewer complications (Malahias et al. 2020), but with more variable results and a reported moderate level of complications at about 9% (Ward et al. 2022; Cooper 2023). The optimal treatment approach remains a topic of ongoing debate. However, novel treatments have emerged in the last decade.
Percutaneous ultrasonic tenotomy (PUT) is a minimally invasive treatment option for plantar fasciitis. PUT entails use of a percutaneous probe that utilizes ultrasound guidance to find pathologic tissue within the plantar fascia and performs a microresection via an 18-gauge needle sized tip that oscillates at a high frequency and emulsifies necrotic tissue. Though there is limited literature on PUT technique for the treatment of tendinopathies, favorable outcomes have been reported for patients with refractory elbow tendinosis (Koh et al. 2013; Barnes, Beckley, and Smith 2015).
PUT was first reported for the treatment of plantar fasciitis in a 2009 retrospective study by Vohra et. al (Vohra and Japour 2009)., who reported significant improvement of American Orthopaedic Foot and Ankle Society (AOFAS) Foot and Ankle rating scores in 41 patients (46 feet) four weeks following the procedure. No complications were reported in this group. A prospective study in 2015 showed significant improvement in AOFAS scores for 11 of 12 patients with refractory plantar fasciitis at 3 months with all patients experiencing relief by 2 years (Patel 2015). Additionally, a larger retrospective review of 107 patients with plantar fasciitis treated with PUT and followed for two years afterwards reported significant improvement in heel pain; 92.5% of patients reported improvement in the pain visual analog scale (VAS) and Foot and Ankle Disability Index (FADI) with 9 patients experiencing mild foot weakness that was successfully improved with orthotics (Iborra et al. 2021). A recent retrospective evaluation of pain VAS in 30 patients either treated with PUT alone or PUT plus platelet rich plasma (PRP) injection reported a significant improvement in VAS pain scores in those treated with PUT and PRP compared to PUT alone (Turner et al. 2023).
Although the literature on PUT for tendinopathies is growing, there is still a paucity of studies investigating the use of PUT for treatment with patients with plantar fasciitis. The aim of this study is to determine the clinical effectiveness of PUT for patients with plantar fasciitis.
Patients and Methods
Institutional review board approval was obtained prior to conducting this study. All information was retrieved from electronic medical records. Data was collected retrospectively from patients who received surgical treatment from the foot and ankle faculty members of an Orthopedic Surgery department between May 2015 and April 2025. Our patient population was identified using the associated ICD-10 (International Classification of Diseases, 10th Revision) for plantar fasciitis/heel pain and 28008, 28060 CPT codes (Current Procedural Terminology) for the plantar fasciotomy procedures. 64 patients were identified who had undergone a plantar fasciotomy. After this initial patient population was compiled, we applied our inclusion criteria: patients 18 years and older with a diagnosis of plantar fasciitis who underwent PUT between the years of 2015 to 2025 at UT Southwestern Medical Center in Dallas, Texas. Pain VAS scores were taken preoperatively (at least one month before the surgery) and postoperatively (at least one month after the surgery). Surveys were conducted by members of the medical team during pre- and post-operative visits. Patients who did not complete pre-operative and post-operative surveys were excluded from the study. After applying our criteria to the sample size, twenty-two patients were identified. We also retrieved additional patient variables including age, gender, body mass index (BMI), and length of follow-up time.
Plantar fasciitis was diagnosed through clinical evaluation and chronic plantar fasciitis/fasciosis was diagnosed with magnetic resonance imaging. Common clinical findings included plantar medial heel pain and pain accentuated with Windless test with a normal neurological exam (no signs of tarsal tunnel syndrome or Baxter’s nerve entrapment). Assessment of foot structure and gastrocnemius equinus were also included in the diagnostic evaluation of plantar fasciitis. Patients who were included in the study failed nonoperative management, which included physical therapy, anti-inflammatories, steroid injections, and night splinting. Patients who had failed nonoperative management were presented with the Tenex procedure as an alternative to conventional surgical treatments. There are several benefits to utilizing Tenex over traditional open surgeries for plantar fasciitis including a minimally invasive approach with a small incision, short surgical time, lower risk of complications, and faster recovery (“Tenex Health- Tenex Health 2025,” n.d.). After reviewing the potential risks and benefits of Tenex, all patients elected to proceed with the procedure.
Data was gathered and the results were analyzed for comparison. All statistical analyses were carried out using SAS 9.4 (SAS Inc., Cary, NC, USA). Descriptive statistics (mean, standard deviation, median, minimum, and maximum) were used for summarizing measurements. The Wilcoxin signed rank test was conducted to compare the pre-operative and post-operative VAS measurements. The level of significance was set at 0.05. 95% confidence intervals for pre-operative and post-operative VAS pain scores, along with Cohen’s d, were calculated to evaluate the reliability of the pain measurements and to quantify the effect size of the treatment. Linear regression analysis was also performed to determine if age, BMI, and gender influenced postoperative outcomes.
Surgical Procedure
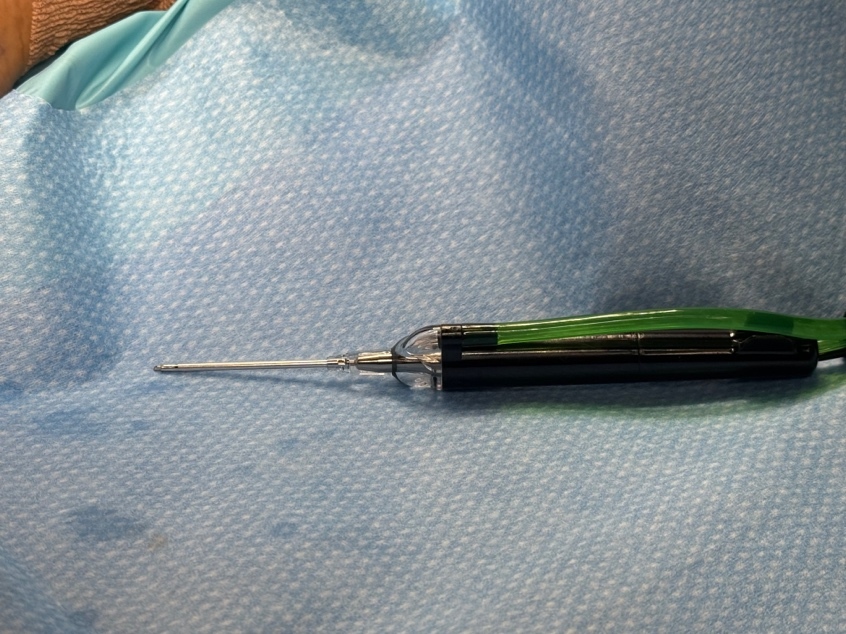
In line with details provided in Turner et al.'s retrospective review study (Turner et al. 2023), the Tenex surgical procedure was outlined as follows. The Tenex Health percutaneous TX MicroTipTM device was used to perform the micro-plantar fasciotomy procedure as seen in Figure 1. All patients received treatment in an outpatient setting. The ultrasound-guided percutaneous micro-plantar fasciotomy procedure was performed in an operating room setting with monitor anesthesia care or general anesthesia. Patients were placed in the supine position with the surgical limb in external rotation. The foot undergoing surgery rested at the end of the examination table. Local anesthesia was administered to the posterior tibial nerve in the tarsal tunnel. The patient’s foot was prepped and draped in the usual aseptic technique.
A 3 mm incision was made medially through the skin at the insertion of the plantar fascial band origin from the plantar medial calcaneal tuberosity of the calcaneus. Diagnostic ultrasound was used to visualize the plantar fascia at its insertion. A hemostat was inserted into the incision and used to bluntly dissect through the subcutaneous tissue to the fascial band. A microtip device and console were set for irrigation, medium aspiration, and medium cutting power. The microtip was inserted into the incision site from the medial heel while using ultrasound visualization of the plantar fascia medial band with both the microtip and the transducer transverse to the plantar fascia.
The microtip is continually passed through the medial band of the plantar fascia and debrided for 3 to 9 minutes as seen in Figure 2. The device was removed from the foot, and the incision was closed with sutures. A non-adherent dressing was placed on the incision site followed by gauze, webril cotton, and an ace bandage. Some patients did receive an injection of PRP to the surgical site after sutures were placed. The patient was fitted with a surgical shoe or short boot walker and was allowed to bear weight as tolerated for the first two weeks. Patients returned to the office two weeks for their first post-operative visit for suture removal; they were then allowed to transition to full weight bearing as tolerated in a supportive shoe. Six weeks after the surgery, patients were instructed with home physical therapy or referred to formal physical therapy.
Results
A total of 22 patients underwent PUT. Demographic information is displayed in Table 1. There were 12 females and 10 males included in the study. The average age and BMI were 54.5 years and 32.4 kg/ m2, respectively. Additionally, within our cohort, 5 patients exhibited pes planus, four with pes cavus, and thirteen demonstrated neutral foot alignment.
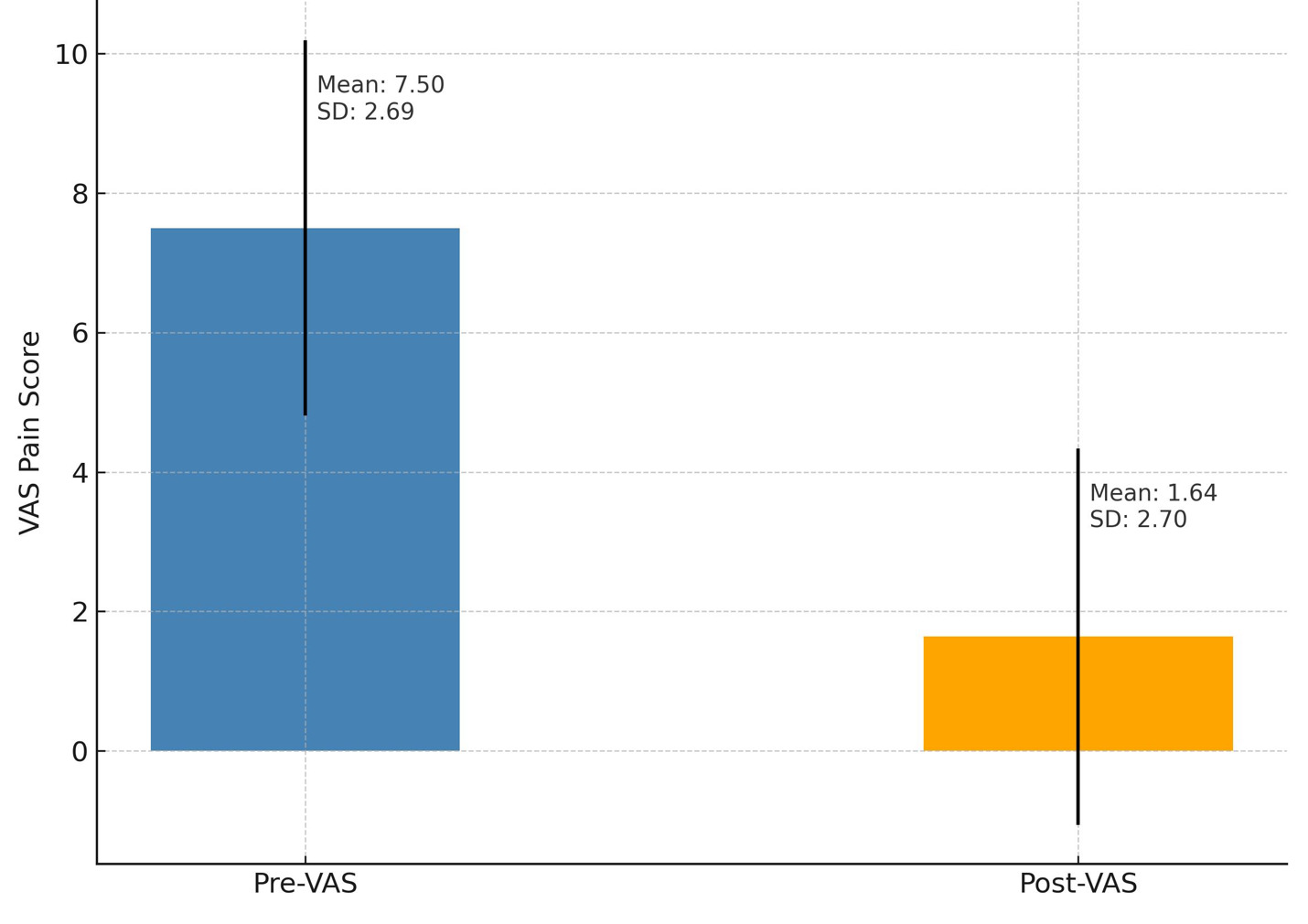
After undergoing the Tenex procedure, patients noted a significant improvement in the VAS scores as demonstrated in Table 2. The pre-operative mean VAS score was 7.50±2.69, whereas the mean post-operative VAS score was 1.64±2.70 at the last follow up (p<0.0001) as displayed in Figure 3. The average follow-up time after surgery was 9.7 months. There were no known complications after the procedure, including infection, bleeding, or delayed healing.
Additionally, 95% confidence intervals (CI) were calculated for pre-operative and post-operative VAS pain scores to help us better understand the potential range of effect sizes, as shown in Table 3. Before treatment with PUT, patients reported moderate to severe pain with pre-operative VAS pain scores falling within a 95% CI of 6.38 to 8.62. Following treatment with PUT, pain levels decreased markedly with post-operative VAS pain scores falling with a 95% CI of 0.51 to 2.77, indicating minimal to mild pain levels. The effect size of the change in VAS pain scores before and after treatment with PUT was also calculated using Cohen’s d. Cohen’s d was found to be 2.17, as illustrated in Table 3. This represents a large effect size, which suggests a clinically and statistically significant improvement in VAS pain scores after PUT.
Linear regression model with the F test was also utilized to determine if demographic factors such as age, BMI and gender influenced change in VAS pain scores. These demographic variables were not significantly associated with a change in VAS pain scores, as demonstrated in Table 4.
Discussion
Plantar fasciitis is a common, persistent cause of heel pain affecting many people in the United States each year. Conservative treatment options, including rest, activity modification, physical therapy, corticosteroid injections, footwear modifications, orthotics, night splints, and shockwave therapy, are utilized initially and often lead to notable improvement in patients with plantar fasciitis pain (Thompson et al. 2014). However, when conservative treatment options fail in a subset of individuals after 6-12 months, different surgical treatments are considered.
PUT has been beneficial in pain relief of a variety of musculoskeletal conditions including epicondylitis of the elbow, insertional Achilles tendinopathy, and tarsal tunnel release (Barnes, Beckley, and Smith 2015; Iborra et al. 2021; Vajapey et al. 2021). There has been a growing number of studies demonstrating the effectiveness of PUT in the treatment of plantar fasciitis (Patel 2015; Vajapey et al. 2021; Pourcho and Hall 2015). Razdan et al. utilized Tenex in 65 patients with recalcitrant plantar fasciitis and observed a greater than 90% improvement in the foot and ankle disability index scores at six-month follow-up (Razdan and Vanderwoude 2015). Higgison et al. conducted a one year follow up study of patients who underwent PUT and reported greater than 90% patient satisfaction, significant reductions in pain, and a high likelihood of patients electing to repeat the procedure, if necessary (Higgison, Wood, and Berkoff 2021). In a newly published study, Encinas et al. similarly demonstrated that PUT was a reliable surgical treatment option for chronic plantar fasciitis with high patient satisfaction and pain relief (Encinas et al. 2025).
Our study findings are consistent with the existing literature. Although our sample size was small, our results demonstrate a marked reduction in VAS pain scores (mean decrease of 5.86 points) and a large effect size (Cohen’s d of 2.17) with PUT treatment of plantar fasciitis. The marked improvement in pain levels at an average follow-up of 9.6 months underscores the sustained effectiveness of the treatment.
Additionally, plantar fasciitis contributes to a significant economic burden in the United States. According to a recent study, the annual cost associated with plantar fasciitis is $284 million (Tong and Furia 2010). Addressing this burden through effective treatment such as PUT can lead to improved outcomes and reduced costs. The PUT procedure is often covered through insurance with costs typically lower than open surgical debridements as noted in one study (Rupe et al. 2023).
There are several limitations in this study. First, due to lack of survey completion of patients, only a small sample size of patients could be included. Second, due to a limited sample size, the study may have been underpowered to detect differences in specific demographic factors associated with VAS pain scores. In future studies, including a larger and more diverse cohort of individuals could help improve the generalizability of findings and increase the statistical power to detect potential associations between demographic factors and treatment outcomes. Third, our study used a single hospital system for patient recruitment, which can lead to selection bias, as the patient population may not be representative of the larger population. Fourth, as with any new technology, the Tenex procedure has a learning curve for surgeons that may impact initial efficiency and patient outcomes as they gain proficiency with ultrasound guidance and device operation. Lastly, we did not observe any documented cases of foot alignment changes (e.g. loss of arch or toe deformities) after the procedure. Subtle alignment changes may have been underreported due to the retrospective nature of the study. Further research studies are also warranted to explore how specific foot morphologies can influence treatment efficacy and long-term recovery.
In conclusion, the findings of this study are encouraging and demonstrate that PUT is an effective treatment option for patients with chronic plantar fasciitis. Given the exploratory nature of the study, the data may lay the groundwork for future large-scale longitudinal studies to further substantiate and build on current results.