Introduction
Prosthetic joint infection (PJI) remains one of the most challenging complications following total hip arthroplasty (THA), with significant implications for patient outcomes. The two-stage revision procedure, which involves temporary removal of the infected prosthesis and placement of an antibiotic-loaded spacer, has become the gold standard for managing chronic PJIs (Lachiewicz, Wellman, and Peterson 2020). This approach allows for local antibiotic delivery and maintenance of joint space while preparing the surgical site for reimplantation.
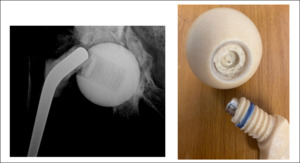
Despite the benefits of this strategy, the use of temporary spacers is not without risk. Mechanical complications, such as spacer loosening, dislocation, and fracture, can lead to increased morbidity and complications of the second stage of the procedure (Craig et al. 2022). These complications are influenced by various factors, including patient characteristics, spacer design, and surgical technique. Articulating pre-formed spacers, such as the OsteoRemedies® REMEDY SPECTRUM® GV antibiotic hip spacer, offer a convenient and effective option for the first-stage of a two-stage exchange. However, data on their mechanical stability remains limited.
The present study aims to evaluate the mechanical stability of the OsteoRemedies® REMEDY SPECTRUM® GV hip spacer in a cohort of patients undergoing two-stage revision for hip PJIs. In this study, mechanical stability refers to both radiographic evidence of component dissociation over time (change in distance between the head and stem) and observed mechanical events such as spacer fracture or dislocation. We assessed associations between mechanical stability and factors including patient comorbidities, application of supplemental bone cement at the head–stem junction, degree of initial threading between components, and postoperative weightbearing status. By identifying factors contributing to spacer failure or success, this study seeks to provide insights into optimizing the use of modular antibiotic spacers in managing PJIs.
Methods
This Institutional Review Board-approved, single-center retrospective study analyzed 18 patients treated by three different orthopaedic surgeons at a Level 1 trauma center. The study included patients who underwent the first stage of two-stage revision arthroplasties for hip prosthetic joint infections (PJIs) between 2020 and 2023, utilizing either the femoral head or stem component, or both, of the OsteoRemedies® second-generation pre-molded antibiotic spacer.
Electronic medical records were reviewed to collect data on patient demographics, comorbidities, infectious organisms, McPherson classification, surgical techniques, spacer components and sizes.
Patient Demographics
Of the 18 patients, there were 10 male and 8 female patients at a mean age of 59 (range: 26 - 79) years. The mean body mass index of our patient population was 29.92 (range: 19 - 47.83) kg/m2. Of the comorbidities assessed in our study, 14 of 18 patients had them (Table 1). According to the McPherson host grade, 1 patient was categorized as IA1, 1 as IB1, 1 as IB2, 1 as IC2, 1 as IIA1, 1 as IIIA1, 4 as IIIA2, 1 as IIIB1, 6 as IIIB2, and 1 as IIIC2 (Coughlan and Taylor 2020).
Of 18 patients, 17 experienced periprosthetic infection according to their calculated pre-op 2018 MSIS score, where a score >/=6, presence of two positive cultures of the same organisms, or sinus tract is consistent with infection (Table 2) (Parvizi, Tan, Goswami, et al. 2018). With a MSIS score of 2 based on only meeting one minor criterion of elevated synovial polymorphonuclear leukocytes, one patient was not classified as having a periprosthetic joint infection as they did not meet any additional minor criteria or either of the two major criteria. There were 14 mono- and 2 polymicrobial infections, with the remaining 2 cases revealing negative cultures. The most commonly identified organisms were Staphylococcus aureus and Staphylococcus epidermidis (Table 2).
The OsteoRemedies® spacer set offers different sizes of the femoral head and stem components to best fit each patient’s unique anatomy, with each size eluting a different amount of gentamicin and vancomycin. The femoral head sizes offered are 46, 54, or 60 mm and the femoral stems come in a short variant with sizes small (111 mm), medium (112 mm), and large (117 mm) or a long variant with sizes small (227 mm), medium (227 mm), and large (231 mm) (OsteoRemedies, n.d.-b). Within our cohort, femoral head sizes used were 46 and 54 mm, while femoral stem sizes used ranged from 111 to 227 mm. All 18 patients used this spacer, with 16 using both the femoral head and stem components and 2 using only the femoral head.
Of the 16 patients who received both spacer head and stem components, 12 were weight-bearing as tolerated (WBAT) and 4 were partial weight-bearing (PWB), including toe-touch weight-bearing (TTWB) and non-weight-bearing (NWB) post-operatively (Table 3). Both patients who experienced spacer fracture or dislocation were WBAT.
Spacer Specifics
Of the 16 patients who used both components, 10 used supplemental bone cement (PMMA) applied around the proximal aspect of the femoral stem, in addition to the MMA liquid monomer which coats the inner surface of the femoral head component to provide fixation between the two components. The remaining 6 patients used only the liquid monomer without the application of external bone cement, which is not the recommended method for maximal fixation.
Each patient used femoral stem and head sizes that best fit their anatomy. The most common femoral stem sizes used were 111 mm with a 54 mm femoral head, followed by 111 mm femoral stem with a 46 mm femoral head (Table 4).
The mean spacer implantation time was 176 days (range: 77-635 days). The mean duration of the most recent follow-up from spacer placement in our cohort was 4 months (1-20 months), where 2 patients had a loss to follow up.
Outcome Variables
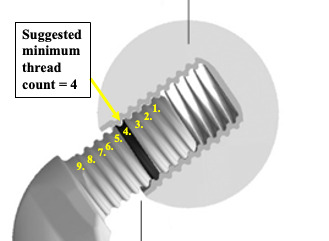
We examined three mechanical stability outcome variables: spacer fracture, dislocation, and dissociation between the head and stem components. A spacer fracture was defined as any break in the femoral trunnion component, the junction between the femoral head and stem. Dislocation was defined as the complete displacement of the spacer head component from the stem. Spacer dissociation refers to any loosening or tightening of the femoral head onto the stem component over time. To measure dissociation, the number of threads on the femoral stem covered by the femoral head, as well as the change in distance between the femoral head and stem, were assessed using post-operative X-rays and most recent follow-up imaging (Figure 1).
Statistical Analysis
Excel sheets was used to run t-tests.
Results
The overall mechanical complication rate was 2/16.
Spacer Fracture
Of the 16 patients who used both femoral components, a spacer fracture occurred in one case (6.25%) (Figure 2). This patient underwent a spacer exchange. Based on initial post-operative x-rays, the degree of threading of the femoral neck into the head was 6 threads, but at the time of fracture, it had reduced to only 2 threads. This patient did not receive additional bone cement, and their BMI was 34.75 kg/m².
The failure pattern involved a fractured polymethyl methacrylate (PMMA) femoral trunnion tip, which was seated at only 2 threads in the femoral head, while the remainder of the femoral stem, including its internal stainless-steel rod, remained intact and dislocated outside of the femoral head socket. This suggests that the femoral head unscrewed from the femoral stem before fracturing.
When comparing this patient who experienced a spacer fracture to another in our cohort with the same thread count of 6 who did not fracture, the key differences between the two patients were the use of supplemental bone cement and BMI of 22.7 kg/m².
Spacer Dislocation
Of the 16 patients who used both femoral components, a spacer dislocation occurred in 1 case (6.25%). In this case, the spacer was exchanged with a different spacer. The degree of threading of the femoral neck into the head was 4 threads. For this patient, additional bone cement was not used, their BMI was 38.02 kg/m², and the patient reported a fall resulting in twisting of the affected limb.
When comparing the demographics of the patient who experienced spacer dislocation to the other patient in our cohort with 4 threads who did not dislocate, the only differences were the use of supplemental cement, BMI 24.4 kg/m², and presence of trauma.
Spacer Dissociation
Among the 16 patients who utilized both components, the femoral head was screwed onto the stem with an average of 7.75 (range: 4–9) threads (Figure 3). The average change in distance between the femoral head and stem components from post-spacer insertion to the most recent follow-up was 0.15 mm (range: -0.5 to 2.93 mm).
Of the 10 patients who used supplemental bone cement around the junction between the femoral stem and head, the average change in distance was –0.15 mm. Of the 6 patients who did not use supplemental cement, the average change in distance was 0.78 mm.
The average change in distance between the spacer head and stem in WBAT patients was 0.33 mm, compared to -0.22 mm in the PWB group. A two-sample t-test comparing WBAT (M = 0.28, SD = 0.86) and PWB (M = -0.22, SD = 0.38) groups showed no statistically significant difference (p = 0.14).
A two-sample t-test comparing the average change in distances between the femoral head and stem in patients who did use supplemental bone cement (M = -0.148, SD = 0.243) versus those who did not (M = 0.784, SD = 1.22) revealed a statistically significant difference (p = 0.0155).
A two-sample t-test comparing the average change in distances between the femoral head and stem in patients whose femoral stem was screwed </= 6 threads into the femoral head recess (M = 0.465, SD = 0.11) versus those whose femoral stem was screwed >/= 6 threads (M = 0.24, SD = 1.23) revealed no significant difference (p = 0.40).
Discussion
Understanding the risk factors associated with mechanical complications of antibiotic-loaded hip spacers is essential, as these complications can significantly impair patient function and compromise outcomes. Although the true incidence and contributing factors remain unclear, a systematic review by Sambri et al. analyzing 1,659 cases reported a 19% rate of mechanical complications in hip spacers, including dislocations and fractures (Sambri, Fiore, Rondinella, et al. 2023). However, there is limited research specifically evaluating the mechanical stability of the OsteoRemedies® modular antibiotic-loaded hip spacer, particularly in relation to risk factors for fracture, dislocation, or dissociation.
This study investigates the outcomes of patients treated with the OsteoRemedies® modular articulating pre-formed hip spacer during the first stage of a two-stage revision arthroplasty at a single institution. The focus is on identifying mechanical complications within this cohort and analyzing associated risk factors.
The OsteoRemedies® spacer is designed for temporary use with an expected lifespan of up to 180 days. According to manufacturer guidelines, proper assembly, which includes securing the modular head onto the stem with a minimum of four threads, is essential for optimal performance. While the use of additional bone cement is recommended, it is not required. Mechanical failure may occur under conditions of excessive load, such as elevated body weight or traumatic events like falls, which may reduce the implant’s fatigue strength and increase the risk of complications (OsteoRemedies, n.d.-a).
In our study, patients who did not receive supplemental bone cement around the junction between the femoral head and stem, applied in a collarette fashion, demonstrated greater radiographic dissociation between components over time compared to those who received cement. Specifically, the average change in distance between the femoral head and stem was significantly greater in the non-cemented group (p < 0.05), suggesting increased micromotion and reduced mechanical stability. Both patients who experienced mechanical complications, including spacer fracture or dislocation, were among those who did not receive supplemental cement. Although these complications were not analyzed statistically as a separate outcome, this observed trend supports the hypothesis that cement augmentation may play a role in maintaining spacer construct integrity during the interim period.
Implanting the spacer without additional cement reflects a press-fit technique that relies on the patient’s native anatomy to stabilize the implant. However, anatomical mismatch between the patient’s anatomy and the spacer may predispose to instability. To mitigate this risk, previous studies have recommended applying a small amount of cement to create a collar around the proximal femoral stem to enhance fixation (Barreira et al. 2015). While several authors suggest that improved mechanical support may reduce complications, direct comparative data evaluating press-fit versus partial or complete cementation techniques for articulating spacers during two-stage revision procedures remain limited (Jung et al. 2009; Faschingbauer et al. 2015).
Another key finding from our study was that the patients in our cohort who experienced spacer fracture and dislocation were both obese (BMI > 30) and did not receive additional supplemental cement at the head-stem junction. Notably, one of the obese patients experienced a traumatic fall during the spacer period. Intuitively, increased body weight, particularly in the absence of supplemental mechanical support, subjects the implant to greater mechanical loads, potentially accelerating wear or failure. Our findings support the hypothesis that obesity and trauma contribute to spacer instability, especially when cement is not used to reinforce the construct.
To further evaluate the influence of thread count, we compared the spacer configurations of patients who experienced mechanical complications to those with the same number of threads who did not. In both matched comparisons, the patients without complications had lower BMIs (22.7 kg/m² and 24.4 kg/m²), received supplemental bone cement, and did not experience trauma, despite having the same thread engagement. These findings suggests that the thread count alone is not likely to be solely responsible for mechanical stability of the spacer. Rather, the interplay of factors, including obesity, absence of supplemental bone cement, and excessive loading from trauma are likely contributing factors to mechanical failure. As such, reliance solely on thread engagement, even when within manufacturer guidelines, may be insufficient to prevent complications in high-risk patients.
Consistent with our observations, Costanzo et al. conducted a study involving 236 patients with periprosthetic joint infection (82 hips and 154 knees) treated with antibiotic spacers (Costanzo, McCahon, Tokarski, et al. 2023). They tracked mechanical complications and performed risk factor analysis, finding that a BMI > 40 was associated with a significantly higher rate of mechanical failure compared to BMI < 40 (42.8% vs. 19.2%, p = 0.013). Although the authors did not stratify outcomes by joint type or exact BMI cutoffs, the results clearly demonstrate that obesity negatively impacts spacer durability.
Further supporting this association, Houdek et. al evaluated outcomes in 99 patients undergoing two-stage revision for hip infection, comparing 33 morbidly obese patients (BMI > 40) to 66 non-obese controls (Houdek, Wagner, Watts, et al. 2015). While the rates of dislocation and loosening were higher in the morbidly obese group, the differences did not reach statistical significance. However, morbidly obese patients had significantly higher overall complication rates (p < 0.001) and revision rates. At 10-year follow-up, 61% of morbidly obese patients required at least one reoperation compared to only 12% of non-obese patients.
Our study has several limitations. First, our focus on one particular spacer implant limits generalizability of the results to other spacers beyond the OsteoRemedies® spacer. Second, our sample size limits our statistical power. Third, the two patients who were lost to follow up may have had complications that we were not aware of, leaving those potential instances unaccounted for. Finally, there were three different surgeons who had unique surgical techniques, so that factor could not be controlled for and may have had an effect on outcomes. However, this is the largest series of OsteoRemedies® hip spacers reported, the dropout rate was only 11%, and the focus on mechanical complications in the context of a limited number of ways these spacers can be assembled and inserted minimizes the influences of different surgeon techniques.
Conclusion
This study highlights the occurrence of mechanical complications, including fracture and dislocation, of OsteoRemedies® hip spacer during the first stage of a two-stage revision.
Patient candidacy should be carefully considered when planning OsteoRemedies® spacer implantation technique. In patients with risk factors highlighted in our study, such as high body mass index (BMI) or excessive loading secondary to trauma, focus should be placed on fixation between the femoral stem and head. To achieve this, surgeons should strongly consider the application of bone cement around the proximal aspect of the femoral stem in a collar-like fashion. Additionally, surgeons should consider patient-specific risk factors to determine the most efficient offset between the femoral head and stem pieces using thread count. Increased fixation between the two components of an articulating hip spacer may prevent mechanical complications of the device.
Future work
Partnering with another institution with patients who used this spacer will make our results more generalizable. Furthermore, this will allow us to further stratify our sample into subgroups such as thread count, BMI > 30, presence of trauma, or weight-bearing status post-operatively to determine if these factors have a significant impact on spacer stability both with and without supplemental cement use.

_between_femoral_head_and_stem_pieces_post-spacer_insert.png)

_between_femoral_head_and_stem_pieces_post-spacer_insert.png)