1. Introduction
Total Knee Arthroplasty (TKA) effectively relieves pain and improves function in advanced knee osteoarthritis, yet postoperative anterior knee pain (AKP) remains a challenge, impacting patient satisfaction and outcomes (Petersen et al. 2014). Patellar management in TKA is widely debated, with surgeons adopting one of three approaches: routine resurfacing, no resurfacing, or selective resurfacing based on patient-specific criteria (McConaghy et al. 2021). Regional variations exist, with resurfacing rates exceeding 80% in the U.S (Abdel, Parratte, and Budhiparama 2014; Fraser and Spangehl 2017)., contrasting with Norway and Sweden (2–4%) (Abdel, Parratte, and Budhiparama 2014; Fraser and Spangehl 2017; Migliorati, Signori, and Silvestrini-Biavati 2012) and Australia (43–59%) favoring selective resurfacing (Fraser and Spangehl 2017; Vertullo et al. 2019; Clements et al. 2010). While resurfacing may reduce AKP and revision rates, studies report no consistent benefits over retention (Cerciello et al. 2016).
As an alternative, patelloplasty reshapes the patella to enhance congruency with the femoral component, involving osteophyte removal and cartilage resection (Cerciello et al. 2016; Antinolfi et al. 2018). Early evidence suggests improved functional scores and patient satisfaction without significant differences in AKP compared to resurfacing (Sun et al. 2012; Župan et al. 2014). A 2012 study reported superior functional scores and satisfaction in patelloplasty patients, with no difference in AKP (Sun et al. 2012), while a 2014 study found improved Knee Injury and Osteoarthritis Outcome Scores (KOOS) and Oxford Knee Scores (OKS), but no significant differences in pain or function (Župan et al. 2014). Patelloplasty also preserves bone stock, allowing future resurfacing if needed (McConaghy et al. 2021).
Despite promising results, patelloplasty lacks standardized techniques, making cross-study comparisons difficult. Since 2004, six studies have found no significant differences between patelloplasty and resurfacing in function, pain, satisfaction, revision, or radiographic outcomes (Burnett et al. 2004; Agarwala et al. 2018; Li et al. 2012; Liu et al. 2012; Hwang, Yang, and Han 2012; Smith, Wood, and Li 2008). Patient factors such as BMI, comorbidities, and patellar morphology influence outcomes, with obesity and diabetes linked to poorer results, while the absence of preoperative fixed flexion deformity predicts better range of motion (ROM) (Lee 2017, 2016).
This study contributes to the growing body of literature by reporting early postoperative outcomes following a consistently applied patelloplasty technique in over 700 knees within a real-world clinical setting. Unlike prior investigations that often lacked standardized surgical protocols or relied on imprecise outcome measures, our analysis quantifies specific functional endpoints and examines how both patient- and procedure-related factors influence recovery. By focusing on mobility, anterior knee pain, and complications, this study aims to clarify the early effects of patelloplasty on post-TKA recovery which can support more personalized and evidence-informed decisions in patellar management during TKA.
2. Methodology
2.1. Study Design and Ethical Compliance
This retrospective, observational cohort study included 408 patients (727 knees) who underwent primary total knee arthroplasty (TKA) with patelloplasty between December 2017 and December 2023 at Tarabichi Joint Care and Tripoli University Hospital, Libya. All clinical data were extracted from electronic medical records collected during routine practice. No patient was contacted or subjected to additional procedures or imaging for research purposes. As such, this study met institutional criteria for exemption from formal IRB approval and was conducted in accordance with the principles of the Declaration of Helsinki. Patient data were fully anonymized prior to analysis, and confidentiality was rigorously maintained throughout.
2.2. Eligibility Criteria and Analytical Approach
Patients were included if they were aged ≥50 years, underwent TKA with intraoperative patelloplasty, and completed both 3- and 6-month follow-up evaluations. Exclusion criteria included incomplete medical records or concurrent confounding orthopedic procedures (e.g., osteotomies, staged revisions).
Each operated knee was considered an independent analytical unit, yielding 727 knees for analysis. For bilateral procedures, outcomes were recorded and analyzed per knee. No statistical adjustments were made for intra-subject correlation, which is acknowledged as a limitation.
2.3. Definition of Functional Outcomes
Clinical endpoints were defined as follows:
-
Full range of motion (ROM): Flexion ≥110°
-
Unaided walking: Ambulation on level ground without assistive devices
-
Stair climbing: Ability to ascend and descend stairs independently
-
AKP: Subjective anterior knee pain reported at follow-up
-
MUA: Requirement for manipulation under anesthesia due to postoperative stiffness unresponsive to physiotherapy
2.4. Surgical Technique
All procedures were performed under spinal anesthesia via a medial parapatellar approach. The patella was everted at 90–100° of flexion. Patelloplasty was executed with the aid of a power-driven oscillating saw blade (1.6–2.2 mm thick, 2.2–2.8 mm wide), and included:
-
Removal of osteophytes, bony bridges, and marginal spurs
-
Surface smoothing with rasps and files to reduce irregularities
-
Vertical excision to correct luxation typically observed between 40°–90° of flexion
-
Horizontal excision to address widened anterior patellar contours or asymmetry
-
Lateral facet trimming in cases of tracking lift-off >5 mm
-
Posterior beveling when indicated for patella baja or asymmetric wear
-
Application of polyethylene patellar components only in cases of severe bone loss
-
Micro-pinning used sparingly in the presence of cysts or peripheral instability
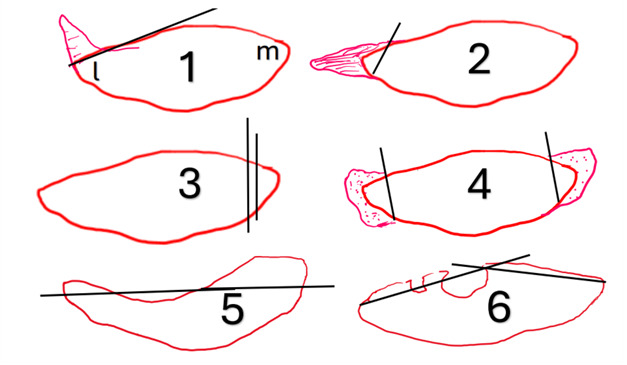
Skyline radiographs at 20° and 40° of knee flexion were used intraoperatively to assess patellar tracking and alignment. Definitions and intraoperative criteria for excision procedures are provided in Figure 1. Postoperative rehabilitation began within 24 hours and included quadriceps activation and passive ROM targeting 90–100° under physiotherapy supervision.
2.5. Data Collection and Variables
Baseline demographic and clinical variables included age, sex, body mass index (BMI: normal [18.5–<25 kg/m²], overweight [25–<30 kg/m²], obese [≥30 kg/m²]), hypertension, diabetes mellitus, osteopenia, and presence of preoperative fixed flexion deformity (10–30°). Osteopenia was assessed via clinical evaluation and radiographic features; dual-energy X-ray absorptiometry (DEXA) was selectively performed based on risk stratification.
Intraoperative data included surgical laterality (unilateral, bilateral simultaneous, bilateral staged), and whether lateral release, vertical excision, or horizontal excision was performed.
2.6. Statistical Analysis
Descriptive statistics (frequencies, means, standard deviations) were computed for all variables. Chi-square and z-tests with Bonferroni correction were used to compare categorical variables. Cramér’s V was applied to determine effect sizes, interpreted as small (<0.1), moderate (0.1–0.3), or large (>0.3).
Multivariable logistic and ordinal regression models were constructed to identify independent predictors of postoperative ROM, functional recovery, and AKP. Predictor variables included patient demographics, comorbidities, deformities, operative approach, intraoperative interventions, and complications (e.g., MUA). Analyses were conducted using SPSS version 26.0, with statistical significance set at p < 0.05. Data visualization was performed using Microsoft Excel.
3. Results
3.1. Surgical Procedure Types and Intraoperative Factors
Bilateral staged TKA was the most common approach (74.0%), followed by unilateral (21.8%) and bilateral simultaneous TKA (4.2%) (Table 2). Intraoperative lateral release was performed in 3.2% of cases, with vertical (1.5%) and horizontal (0.5%) excisions being less frequent.
3.2. Functional Outcomes
At 6 months, 86.0% achieved full ROM (≥110° flexion), with ROM up to 70°, 100°, and 110° observed in 4.9, 3.9, and 5.1%, respectively. Walking unaided improved from 74.0% at 3 months to 77.9% at 6 months, though 15.1% of patients regressed. Conversely, 71.3% of those unable to walk unaided at 3 months regained mobility. Stair climbing improved from 66.0% to 72.1%, with 95.4% of initially impaired patients recovering, while 27.0% of those previously capable regressed (Table 3).
3.3. Post-Operative Complications
AKP incidence declined from 8.8% at 3 months to 2.7% at 6 months (Table 3). MUA was required in 3.2% of cases. MUA was required in 13 patients (3.2%) who experienced postoperative stiffness unresponsive to physiotherapy. All MUA procedures were performed within 3 months of surgery.
3.4. Associations Between Patient Characteristics and Outcomes
Female gender had a higher likelihood of walking unaided at 3 months (OR=4.313, 95% CI=[2.663, 6.986]) than male gender, Females also had higher AKP prevalence (OR=4.254, 95% CI=[1.730, 10.462]).
Post-operative anterior pain was of a higher percentage among Obese patients at 3 months (Cramér’s V=0.406) and 6 months (Cramér’s V=0.231). Patients with pre-operative 10–30° fixed flexion had a higher percentage of those who could climb stairs at 3 months (OR=1.82, 95% CI=[1.16, 2.84]) and lower percentage of post operative anterior pain (Table 5). Diabetics had higher percentage of post-operative pain at 3months (OR=2.73, 95% CI=[1.36, 5.45]) and 6 months (OR=4.04, 95% CI=[1.16, 14.05]), while osteopenic patients showed improved stair climbing (OR=2.08, 95% CI=[1.057, 4.09]) but higher pain at 6 months (OR=3.4, 95% CI=[0.967, 12]) (Table 5). Effect sizes for categorical variables were interpreted as small (Cramér’s V < 0.1), moderate (0.1–0.3), or large (>0.3) (Cohen 2013).
3.5. Predictors of Post-Operative Outcomes
Multivariable regression showed that the absence of pre-operative fixed flexion deformity (OR=2.23, 95% CI=[1.24, 4.03]) and being a man (OR=1.87, 95% CI=[1.01, 3.47]) predicted better ROM (Table 6). Women were more likely to walk unaided at 3 months (OR=4.43, 95% CI=[2.72, 7.23]), while MUA negatively impacted this outcome (OR=0.30, 95% CI=[0.09, 0.98]). Ordinal regression confirmed that being a man and the absence of pre-operative fixed flexion deformities were associated with better ROM outcomes.
4. Discussion
This study evaluated whether patelloplasty in total knee arthroplasty (TKA) is associated with anterior knee pain (AKP), functional recovery, and postoperative complications. Patelloplasty — reshaping the native patella rather than retaining or resurfacing it — aims to enhance patellofemoral congruency while mitigating complications associated with traditional patellar management strategies (Sonkusale and Phadnis 2024; Habib, El Dsh, and Dewidar 2024; De Padua et al. 2024). In this retrospective analysis of 408 patients (727 knees), we observed a reduction in AKP from 8.8% at 3 months to 2.7% at 6 months. Functional recovery also improved, with 86.0% of knees achieving full ROM (≥110°), and over 70% of patients regaining stair-climbing ability. The complication rate was low, with only 3.2% requiring manipulation under anesthesia (MUA).
These findings align with previous literature indicating that patelloplasty may reduce AKP and enhance mobility when compared to traditional patellar retention techniques (Župan et al. 2014; De Padua et al. 2024). Župan et al. reported improved functional outcomes and pain relief with patelloplasty compared to conventional methods (Župan et al. 2014), while De Padua et al. found its results comparable to patellar resurfacing, positioning it as a bone-preserving alternative (De Padua et al. 2024).
Our 6-month functional outcomes—86.0% achieving full ROM, defined as flexion of ≥110°, 77.9% walking unaided, and 72.1% climbing stairs—mirror or exceed published benchmarks (Župan et al. 2014; Feng et al. 2023). Similarly, our low complication rate is consistent with literature supporting patelloplasty as a safe approach with reduced revision or MUA needs (De Padua et al. 2024).
While meta-analyses suggest resurfacing may reduce AKP compared to retention (OR ~1.84) (Simpson et al. 2023), patelloplasty appears to deliver comparable clinical benefits while avoiding prosthetic-related complications (De Padua et al. 2024). From a biomechanical standpoint, reshaping the patella can improve tracking, reduce focal contact pressures, and enhance stress distribution—potentially lowering AKP incidence (De Padua et al. 2024). It also preserves bone stock, reduces fracture risk, and may facilitate future revision in younger patients or those with atypical patellar morphology (De Padua et al. 2024; Kedia 2022).
The lack of technique standardization remains a key limitation in current literature (De Padua et al. 2024). In our cohort, consistent intraoperative correction of trochlear mismatch and peripheral trimming may have contributed to favorable outcomes. This underscores the need for establishing reproducible, widely adopted surgical protocols.
Registry data further suggest that, when using patella-friendly implants, differences in AKP between resurfacing and non-resurfacing strategies diminish (McConaghy et al. 2021; Kedia 2022). Patelloplasty may be particularly beneficial for patients with anatomical complexity or those in resource-constrained environments. Economically, it may reduce implant costs and complication-driven revisions (McConaghy et al. 2021; Kedia 2022).
Our findings are also in line with literature suggesting that patelloplasty can offer lasting improvements in ROM and satisfaction, especially for patients with irregular patellar morphology (Feng et al. 2023; Kedia 2022). Though this study captured outcomes only through the 6-month mark, the positive functional trajectory supports the hypothesis that long-term durability is likely.
Regarding patient-reported outcomes (PROMs), previous studies using KOOS and OKS have shown minimal differences between patelloplasty and resurfacing (De Padua et al. 2024; Kedia 2022). PROMs were not uniformly collected in our cohort, but functional outcomes were consistently documented through predefined clinical assessments.
Patient-specific variables influenced recovery: obesity and diabetes correlated with higher AKP, in line with previous reports (Feng et al. 2023), likely reflecting biomechanical loading and delayed healing. Interestingly, women were more likely to report AKP but also regained ambulation sooner, reinforcing the multifactorial nature of recovery trajectories.
While these findings are promising, several limitations must be acknowledged. This was a retrospective, observational study lacking a comparator cohort (resurfaced or retained patellae), which limits the strength of causal inferences. Additionally, range of motion was recorded by trained clinicians using angle-based categories, but inter-rater reliability was not formally tested. PROMs such as the KOOS, OKS, or VAS were not administered systematically, precluding direct comparison with validated patient-centered instruments. Finally, follow-up was limited to 6 months, which may not capture delayed complications or long-term durability. These limitations underscore the need for prospective, randomized trials with standardized outcome measures and longer follow-up, as emphasized in prior studies of long-term TKA outcomes and radiological comparisons (Eshnazarov, Seon, and Song 2016; Chun et al. 2017).
In conclusion, while causality cannot be established due to the absence of a comparator group, our findings suggest that patelloplasty may support early postoperative recovery following TKA by reducing AKP, improving ROM, and preserving function—all with low complication rates. When performed with precise intraoperative reshaping, the technique may offer a viable middle ground between retention and resurfacing strategies. Nevertheless, further prospective studies with validated PROMs, longer follow-up, and comparative cohorts are essential to confirm the long-term value and generalizability of patelloplasty in TKA.


_and_post-operative_(bottom_row)_skyline_radiographs_at_30_knee_fl.png)
_walking_flat_unaided_and_(b)_walking_up_down_stair.png)
_and_post-operative_(bottom_row)_skyline_radiographs_at_30_knee_fl.png)
_walking_flat_unaided_and_(b)_walking_up_down_stair.png)