INTRODUCTION
Femoroacetabular impingement (FAI), a common cause of hip pain, was initially identified by Ganz et al (Ganz et al. 2003). in 2003, and has a prevalence of 54.5 per 100,000 persons. Typical patients who present with FAI are younger (18-35 years) and physically active (Hale et al. 2021). Since the discovery of FAI, there has been a significant increase in the use of hip arthroscopy to treat this condition (Sing et al. 2015; Montgomery et al. 2013). Indications for hip arthroscopy have been increasing over the past decade, with FAI and labral tears being among the most common (Scanaliato et al. 2022; Maldonado et al. 2022; Mowers et al. 2025). FAI is associated with three types of bone deformities: cam lesions, which form a bony prominence at the head and neck region of the femur; pincer lesions, which form at the acetabular rim causing an overhang of the acetabulum; and a mixed lesion that has elements of both cam and pincer lesions (O’Rourke and El Bitar 2024). Each lesion may cause impingement of the labrum and cartilage, particularly with motion of the joint.
Hip arthroscopy techniques for FAI include both femoroplasty and acetabuloplasty (Byrd and Jones 2009; Redmond et al. 2015). In both techniques capsulotomy, where the iliofemoral ligament is cut to gain access to the hip compartments, may be performed to allow for improved visualization. Closure of the capsule after capsulotomy in hip arthroscopy is at the discretion of the surgeon; however, there is an increasing number of studies that indicate capsular closure may lead to greater hip stability, and therefore, better clinical outcomes than leaving the capsule unrepaired (I. K. Bolia et al. 2019; Dasari et al. 2023; Sugarman et al. 2021). Capsular closure can be achieved through side-to-side repair or capsular shift repair; either technique may include capsular plication (De Giacomo et al. 2021). In each case, absorbable or nonabsorbable sutures are used to close the capsule and recreate native anatomy. While capsular closure has been shown to help combat hip instability, it is currently unknown whether the suture material used to close the capsule imparts a significant effect on post-operative stability (I. Bolia, Briggs, and Philippon 2018; Di Benedetto et al. 2020). Generally, each suture type provides distinct advantages and disadvantages in capsular closure. Absorbable sutures provide temporary support and eliminate the need for removal but may provoke more superficial inflammation and lose tensile strength over time (Pillai and Sharma 2010; Yag-Howard 2014; Moy, Waldman, and Hein 1992; Bennett 1988). Non-absorbable sutures offer durable tensile strength beneficial for long-term stability, but they can increase the risk of soft tissue irritation or foreign body reaction (Yag-Howard 2014; Moy, Waldman, and Hein 1992; Bennett 1988).
There is little information in the literature regarding whether the use of absorbable versus nonabsorbable sutures for capsular closure can impact outcomes following hip arthroscopy for FAI. Therefore, the purpose of this review was to investigate outcomes of absorbable versus non-absorbable sutures for capsulotomy closure during hip arthroscopy for the treatment of femoroacetabular impingement syndrome. We hypothesized that there would be no difference in outcomes following hip arthroscopy with capsule closure for FAI using absorbable vs nonabsorbable sutures.
METHODS
Search Strategy and Eligibility Criteria
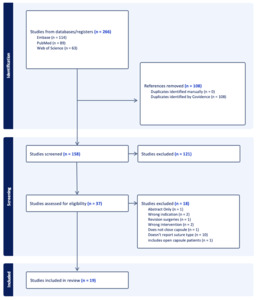
In accordance with guidelines set by the 2020 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement (Page et al. 2021), a complete search of the existing literature was conducted. PubMed, Embase, and Web of Science databases were queried in September 2024 using the following MeSH string: (hip) AND (arthroscopy) AND ((femoroacetabular impingement syndrome) OR (FAI)) AND ((Capsule) OR (capsular)). Studies met inclusion criteria if included patients underwent hip arthroscopy with capsule closure for a primary diagnosis of femoracetabular impingement syndrome with a minimum two-year follow-up. Exclusion criteria included abstracts, non-English language studies, editorial articles, surveys, biomechanical/cadaveric/animal/in vitro studies, technique papers, review articles, and case reports.
Abstract and full-text screening of each article was performed by two independent authors (JC and CM). No discrepancies between the authors occurred. If studies shared identical or similar author lists and were determined to likely be using the same patient cohort upon close inspection, the latest publication or publication with the largest cohort was utilized to ensure the same patient cohort was not included multiple times.
Data Extraction
Data were extracted from the included studies by two independent authors (JC and CM) and entered into a Microsoft Excel (Version 16.67; Microsoft Corp., Redmond, WA) spreadsheet. Data collection included first author’s name, date of publication, Level of Evidence (LOE), patient demographics, mean follow-up time, suture type used for capsule closure (absorbable vs non-absorbable), capsule closure technique, as well as the delta (change from preoperative to postoperative) for patient report-outcome measures (PROMS) were recorded. The PROMS included the modified Harris Hip Score (mHHS), and Hip Outcome Score (HOS). Post-operative complication and revision rates were also collected.
Risk of Bias Assessment
The Methodological Index for Non-Randomized studies (MINORS) criteria (Slim et al. 2003) was utilized by two independent authors (JC and CM) to conduct a quality assessment of the included studies (Appendix 1). Each ranking for an included study was compared and no difference was identified between the authors. To score noncomparative, nonrandomized studies, the MINORS criteria utilized a scale with a maximal score of 16 points. Each criterion that makes up the MINORS grading system is scored based on the quality of reporting: 0 if not reported, 1 if reported but inadequate, or 2 if reported and adequate. The Revised Cochrane Risk of Bias (ROB 2) tool (Higgins et al. 2011) was utilized for bias assessment among randomized controlled trial(s). The tool, which categorizes bias into five domains (D1, D2, D3, D4, D5), assigns studies one of three levels of risk of bias: low risk, unclear risk, and high risk (Appendix 2).
Statistical Analysis
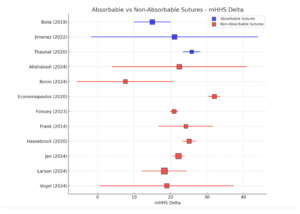
Due to the heterogeneity of the data included as well as an overall low Level of Evidence among studies, pooling of data was avoided. Descriptive statistics were employed for statistical analyses of pre- and post-operative outcomes between absorbable and non-absorbable suture groups. The delta, change from preoperative to postoperative outcome values, were reported and qualitatively compared. One-armed forest plots were created using Python Maplotlib & Statsmodels (Version 3.12, Python Software Foundation, Delaware, US), to display the deltas from each patient-reported outcome measure (PROM) in which three or more studies reported mean ± standard deviation for the respective PROM.
RESULTS
The initial search of the existing literature identified 266 studies, of which 108 duplicate articles were removed (Figure 1). Following abstract screening, there remained 37 articles that were eligible for full-text screening. After full-text screening was performed, 19 articles published from 2014 to 2024 reporting on a total of 1,740 patients (1,745 hips) met the final inclusion/exclusion criteria. The overall mean MINORS score was 20.1 (range, 18-22) for comparative studies and 11.0 (range, 10-12) for non-comparative studies (Appendix 1). The Cochrane Risk of Bias 2 (RoB 2) tool revealed a low risk of bias among the two included randomized controlled trials (Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020). Six studies (I. K. Bolia et al. 2019; Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Thaunat et al. 2020; Beals et al. 2022) reported on capsular repair using absorbable suture material, while thirteen studies (Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Filan and Carton 2020; Foissey et al. 2023; Frank et al. 2014; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Okanoue et al. 2023; Della Rocca et al. 2022; Soriano et al. 2023; Vogel et al. 2024) reported on capsular closure using nonabsorbable sutures.
Demographics
Of the 1,740 patients included in this study, 406 patients with a mean age of 33.4 years (mean range, 28.5-41.0 years) underwent capsular closure with absorbable sutures while 1,334 patients with a mean age of 29.9 years (mean range, 18.6-36.0 years) underwent capsule closure with nonabsorbable sutures (Table 1). Mean follow-up of the absorbable suture group was 91.2 months (mean range, 40.4-144.0 months), while the mean follow-up of the nonabsorbable suture group was 57.5 months (mean range, 24-121.2 month
Labral lesions were reported in four studies (Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Beals et al. 2022) in the absorbable suture group and twelve studies (Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Foissey et al. 2023; Frank et al. 2014; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Okanoue et al. 2023; Della Rocca et al. 2022; Soriano et al. 2023; Vogel et al. 2024) in the nonabsorbable suture group and occurred in 97.1%-100% and 74%-100% of patients, respectively (Table 1). Tonnis classification was reported by five (I. K. Bolia et al. 2019; Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Thaunat et al. 2020) absorbable suture studies and nine (Bonin, Manzini, and Viamont-Guerra 2024; Allahabadi et al. 2024; Filan and Carton 2020; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Okanoue et al. 2023; Della Rocca et al. 2022; Vogel et al. 2024) nonabsorbable suture studies. Alpha angle was reported in three (I. K. Bolia et al. 2019; Domb et al. 2024; Jimenez et al. 2022) absorbable suture studies with a mean of 62.2° (range, 38°-90°). In the nonabsorbable suture studies, alpha angle was reported by eleven studies (Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Filan and Carton 2020; Foissey et al. 2023; Frank et al. 2014; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Okanoue et al. 2023; Soriano et al. 2023; Vogel et al. 2024) with a mean of 62.9° (range, 40°-90°). Lateral center-edge angle (LCEA) demonstrated a mean of 30.9° (range, 20.0-48.0°) in four absorbable suture studies (Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Beals et al. 2022), while all thirteen nonabsorbable suture studies reported LCEA with a mean of 31.4° (range, 20.0°-43.0°).
The most common concomitant procedure in the absorbable suture studies was labral repair (68.5%, n=278 patients), while the most common concomitant procedure in nonabsorbable suture studies was femoroplasty (69.9%, n=932 patients) (Table 2). An anterolateral approach was the most commonly used arthroscopic portal site for both cohorts, utilized by 5 (5/6, 83.3%) absorbable and 12 (12/13, 92.3%) nonabsorbable studies, followed by a mid-anterior approach, used in 4 (4/6, 67.7%) and 5 (5/13, 38.5%) studies, respectively. Interportal capsulotomy was the most commonly performed capsulotomy, with five (5/6, 83.3%) absorbable and six (6/13, 46.2%) nonabsorbable studies doing so. T-type capsulotomy was performed by one (1/6, 16.7%) absorbable study and six (6/13, 46.2%) nonabsorbable studies.
Patient Reported Outcome Measures
The delta modified Harris Hip Score (mHHS) ranged from 0-30.3 (n=5 studies [I. K. Bolia et al. 2019; Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Thaunat et al. 2020]) in the absorbable suture group compared to 7.6-32.0 in the nonabsorbable group (n=11 studies [Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Filan and Carton 2020; Foissey et al. 2023; Frank et al. 2014; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Okanoue et al. 2023; Vogel et al. 2024]) (Table 3 & Figure 2). The delta HOS-Sport ranged from 31.0-37.2 (n=3 studies [I. K. Bolia et al. 2019; Domb et al. 2024; Jimenez et al. 2022]) in the absorbable suture group versus 28.0-48.3 (n=10 studies [Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Frank et al. 2014; Hassebrock et al. 2020; Jan et al. 2024; J. H. Larson et al. 2024; Della Rocca et al. 2022; Soriano et al. 2023; Vogel et al. 2024] ) in the nonabsorbable suture group (Figure 3).
Postoperative Complication and Revision Rates
Postoperative complication rates in the absorbable suture group ranged from 0% to 10.7% versus to 0% to 31.8% in the nonabsorbable suture group (Table 4). Commonly reported complications in the absorbable group included adhesions (2.0%, n = 8 patients), capsular defects (0.2%, n = 1 patient), and labral insufficiency (0.2%, n = 1 patient). In the nonabsorbable suture group, the most reported complications were worsening symptoms (0.4%, n = 6 patients) and transient pudendal neuropathy (0.2%, n = 3 patients).
Revision rates ranged from 0% to 15.9% in the absorbable suture group (n=5 studies [I. K. Bolia et al. 2019; Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Beals et al. 2022]) versus 0% to 14.9% in the nonabsorbable suture group (n=11 studies [Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Filan and Carton 2020; Foissey et al. 2023; Frank et al. 2014; Hassebrock et al. 2020; J. H. Larson et al. 2024; Della Rocca et al. 2022; Soriano et al. 2023; Vogel et al. 2024]). Conversion to total hip arthroplasty (THA) ranged from 0% to 23.7% in the absorbable suture group (n=6 studies [I. K. Bolia et al. 2019; Atzmon et al. 2019; Domb et al. 2024; Jimenez et al. 2022; Thaunat et al. 2020; Beals et al. 2022]) versus 0% to 17.4% in the nonabsorbable group (n=9 studies [Bonin, Manzini, and Viamont-Guerra 2024; Economopoulos, Chhabra, and Kweon 2020; Allahabadi et al. 2024; Filan and Carton 2020; Foissey et al. 2023; Frank et al. 2014; J. H. Larson et al. 2024; Soriano et al. 2023; Vogel et al. 2024]).
DISCUSSION
The primary findings of our study demonstrated that absorbable suture material for hip capsular closure showed comparable outcomes and revision rates with lower rates of complications when compared to nonabsorbable suture following hip arthroscopy for femoracetabular impingement syndrome. Additionally, we found conversion to total hip arthroplasty (THA) ranged from 0% to 23.7% in the absorbable suture group versus 0% to 17.4% in the nonabsorbable group. However, it is important to note that this could be due to the longer follow-up in the absorbable group (91 vs 58 months), and is likely unrelated to suture type.
When choosing between absorbable and non-absorbable sutures for hip capsule closure, it is important to consider both the healing timeline of the capsule and the suture’s duration of tensile strength. Absorbable sutures typically lose all their tensile strength within two to three months after implantation (Bourne et al. 1988; Müller, Snedeker, and Meyer 2016). This characteristic can be advantageous as it eliminates any foreign material, such as residual knots, which might otherwise cause irritation or mechanical symptoms over time (Al-Mubarak and Al-Haddab 2013). However, complications like adhesions and capsular defects in the absorbable suture group may be linked to the degradation of the material, potentially disrupting the healing process. Studies on absorbable implants, such as screws, have shown similar issues with delayed healing and required reoperations, suggesting that the degradation of absorbable suture material may contribute to these complications (Kramer et al. 2020; Laupattarakasem et al. 2014).
In contrast, non-absorbable sutures maintain their tensile strength throughout the entire recovery period, potentially offering more robust support for the healing capsule (Khalid and Billa 2023). A systematic review by Heifner et al (Heifner et al. 2024). showed a trend toward increased use of T-type capsulotomy and varied closure techniques in hip arthroscopy, with both absorbable and nonabsorbable sutures being used in similar proportions. A retrospective cohort analysis by Moore et al (Moore et al. 2024). found capsular closure with absorbable sutures was equally effective as closure with non-absorbable sutures following hip arthroscopy for FAI. Similar to the present study, they found slightly higher rates of complications in the nonabsorbable suture sub-group. Another study by Lv et al (Lv et al. 2024). found that capsule closure in hip arthroscopy is associated with lower rates of conversion to THA. While the results of this systematic review did not demonstrate a difference in conversion to THA rates, perhaps due to differences in follow-up length between the two cohorts, the higher tensile strength of nonabsorbable suture material may provide a lower risk of capsular closure failure (Bourne et al. 1988; Müller, Snedeker, and Meyer 2016). Thus, it is likely that nonabsorbable suture material could provide lower rates of conversion to THA as a capsular closure failure would perform similarly to an unrepaired capsule.
However, there is no agreement in the literature on whether the hip capsule should be routinely closed after arthroscopic hip procedures (Bindi et al. 2024; Mortensen et al. 2021). A randomized controlled trial (RCT) by Bonin et al (Bonin, Manzini, and Viamont-Guerra 2024). in 2024 showed that there were no significant differences in clinical outcomes between patients undergoing hip arthroscopy with or without capsular closure. Similarly, another RCT by Bech et al (Bech et al. 2023). concluded that there is no clear benefit to routinely performing capsular closure after inter-portal capsulotomy during hip arthroscopy, as both approaches led to similar improvements in pain and function. These two RCTs suggest that the decision to close the capsule — and thus the choice of suture material — may be more dependent on surgeon preference and patient-specific factors rather than clear evidence-based, one-size-fits-all guidelines. For example, some studies have shown capsular closure may be more indicated in patients with generalized ligamentous laxity, hip dysplasia, and competitive athletes (Hassebrock et al. 2020; C. M. Larson et al. 2015; Krych et al. 2016; C. M. Larson et al. 2016; Chandrasekaran et al. 2017; Domb, Chaharbakhshi, Perets, Yuen, et al. 2018). One study found that complete capsular closure after hip arthroscopy was associated with a faster return to play and a higher rate of return compared with that of non-closure of the capsule in this sample population of high-level athletes (Hassebrock et al. 2020). At a minimum 2-year follow-up, complete capsular closure was associated with significantly higher patient-reported outcomes compared with those of non-closure in athletes who underwent hip arthroscopy.
On the other hand, routine capsular closure after primary hip arthroscopy is gaining favor as emerging evidence highlights the drawbacks of leaving the capsulotomy unrepaired (I. K. Bolia et al. 2019; C. M. Larson et al. 2016; Domb, Chaharbakhshi, Perets, Walsh, et al. 2018). Especially in the setting of FAI, recent studies have shown that complete capsular closure can lead to significantly better functional outcomes, including improved sports-specific performance and reduced rates of revision surgery (Tahoun et al. 2023). Economopoulos et al (Economopoulos, Chhabra, and Kweon 2020). demonstrated that at two-year follow-up, patients in the capsular closure group experienced significantly better HOS-ADL, HOS-Sport, and mHHS scores over a two year interval compared to those in the unrepaired T-capsulotomy group. Furthermore, none of the patients in the repaired group required THA, whereas four patients from the unrepaired T-capsulotomy group underwent THA. More pertinent to our study, Frank et al (Frank et al. 2014). compared the clinical outcomes of hip arthroscopic surgery with T-capsulotomy using either partial capsular repair (PR) or complete capsular repair (CR) in patients with FAI. Their findings suggested that patients undergoing complete capsular repair may obtain better sport-specific outcomes, higher patient satisfaction, and lower revision rates than those who received partial repair.
Despite these findings, several factors beyond suture type may impact the outcomes of capsular closure following hip arthroscopy. The number of throws, number of sutures, knotting technique, and suture size, type, and density can also significantly affect the success of capsular repair for FAI. Notably, suture type is often underreported in studies, and when it is included, the reporting is inconsistent (Heifner et al. 2024). A study by Chahla et al (Chahla et al. 2017). found that the biomechanical strength of two or three sutures was significantly stronger than that of one suture. Additionally, a study by Murata et al (Murata et al. 2022). found that the choice of suturing technique can greatly influence hip stability post-surgery. Specifically, they compared standard suturing techniques and newer techniques like the shoelace and Quebec City Slider (QCS) methods. These studies suggest that along with the absorbability of the suture, selecting the appropriate suturing method, along with the number of sutures used for closure is crucial for achieving optimal outcomes in hip arthroscopy, particularly when dealing with large capsular incisions. There is a paucity of research investigating the number of throws and suture size and density affecting capsule closure.
Lastly, how the capsule is closed during hip arthroscopy can significantly influence patient outcomes, and several techniques are commonly used. The two main methods of capsular closure are the T-capsulotomy closure and the inter-portal capsulotomy closure. In a T-capsulotomy closure, a vertical incision is made through the capsule, and closure involves suturing both the vertical and horizontal limbs of the “T” using techniques like simple interrupted or figure-of-eight sutures. The inter-portal capsulotomy closure, on the other hand, involves suturing the capsule between the anterolateral and anterior portals, often using a side-to-side or running suture technique to close the incision. A study by Tahoun et al (Tahoun et al. 2023). found that while both closed and open capsular techniques improve functional outcomes after hip arthroscopy for FAI and labral tears, complete capsular closure may lead to better long-term sport-specific outcomes. However, the overall long-term benefits between the two approaches may be similar, as both groups showed comparable rates of achieving minimal clinically important difference (MCID) and reoperation rates over a 5-year follow-up.
Future research should focus on high-quality, prospective studies directly comparing absorbable and non-absorbable sutures to determine their impact on hip stability, capsular healing, and long-term outcomes. Both clinical and non-clinical studies evaluating suture characteristics – such as size, knotting technique, and number of throws – and their influence on capsular integrity are also needed. Additionally, standardized reporting of suture type and closure technique would help guide evidence-based best practices for capsular repair in hip arthroscopy.
Limitations
Our study is not without limitations, some of which are inherent to systematic reviews. First, there is a lack of randomized controlled trials specifically comparing absorbable and non-absorbable sutures, which limits the strength of the conclusions that we can draw. Due to the limited amount of data, the authors made every effort to ensure that there were no overlap between cohorts investigated by included studies. Each study that met inclusion criteria and possessed similarities in the author last was compared to ensure large enough differences in the participant demographics and data collection timeline to reasonably suspect that separate cohorts were analyzed with no overlap. Additionally, there was a large difference in the number of patients identified for absorbable and nonabsorbable suture cohorts. The studies included in this review also had varying levels of evidence and methodologies, leading to potential heterogeneity in the results. There is also an inconsistency in reporting suture characteristics, such as suture size, knotting technique, and the number of sutures used, which may influence outcomes but were not uniformly documented across studies. The follow-up duration was notably longer in the absorbable suture group compared to the nonabsorbable suture group, with a mean difference of 33.7 months (91.2 months in the absorbable group and 57.5 months in the nonabsorbable suture group). The difference in follow-up duration between the two groups could impact the results by allowing more time for complications or recurrences to be detected in the absorbable suture group, potentially skewing the comparison of outcomes. Finally, selection bias could be present, as the decision to use absorbable or non-absorbable sutures is often based on surgeon preference potentially affecting the generalizability of the results.
CONCLUSION
The use of absorbable suture material for capsular closure in hip arthroscopy for femoroacetabular impingement syndrome demonstrates comparable outcomes and revision rates, with potentially lower complication rates compared to nonabsorbable sutures.