Introduction
Total knee arthroplasty (TKA) is routinely performed as the only curative treatment for osteoarthritis. Severe bone and soft tissue loss from rheumatoid arthritis, post-traumatic arthritis, oncologic resection, infection, fracture, or revision TKA may require an implant design with greater constraint for valgus/varus stability (Dall’Oca et al. 2017). For example, a condylar constrained knee (CCK) implant has more medial-lateral stability by using a larger cam-post mechanism. Current literature generalizes the limitation of CCK through the lens of severe bone loss and complete ligamentous instability and a rotating hinge is necessary when no other implant design would allow for a functional prosthesis (Sabatini et al. 2017; Pasquier, Ehlinger, and Mainard 2019; Kouk et al. 2018). However, modern developments in biological fixation, such as metaphyseal sleeves (DePuy), Cones (Multiple companies), and Optistems (Waldemar Link) blur the exact indications for conversion to rotating hinge more than in the past (Zitsch et al. 2024).There is a paucity of data on CCK vs rotating hinge in general and even less data under various clinical conditions. Nonrandomized data suggests no difference in outcomes, further obscuring the optimal indication for converting CCK to rotating hinge (Kouk et al. 2018; Zitsch et al. 2024).
This clinical opinion article aims to describe an algorithm for a surgeon to decide between a CCK and rotating hinge implant in complex and revision TKA.
Condylar Constrained Knee vs. Rotating Hinge Knee
A CCK uses a taller and more rectangular post to stabilize the knee joint against valgus/varus and torsional forces; this shared load between the implant mechanisms and soft tissue has been shown to increase rates of aseptic loosening at the bone-implant interface (Sabatini et al. 2017). Modern developments in bone augmentation such as metaphyseal cones and sleeves (Zimmer Biomet, Stryker Orthopedics, DePuys Synthes, Smith + Nephew) along with OptiStem (Waldemar Link) are designed to increase the metal-bone interface fixation of the CCK and hinge implant (Zitsch et al. 2024; Heidenreich et al. 2022; Sheth, Bonadio, and Demange 2017).
A hinge knee implant is the maximum constraint a knee prosthesis can provide, using a mechanical component to attach the femur to the tibia and is not reliant on a functional medial and lateral collateral ligaments (Pasquier, Ehlinger, and Mainard 2019). First generation designs lacked rotation and data showed unacceptably high rates of complications such as fracture and patellar maltracking issues (Barnoud et al. 2021). Second generation rotating hinge knees improved outcomes by adding a rotational component and restoring some knee kinematics (Barnoud et al. 2021).
Kouk et al. reviewed postoperative complications with rotating hinge in revision TKA, finding infection and loosening were the most common adverse events (Kouk et al. 2018). Jones et al. reviewed two case series of thirty patients and found patellar complications occurred with hinge knee implants (Jones, Barrack, and Skedros 2001). Biological fixation through metaphyseal sleeves had no cases of loosening at a mean follow-up time of forty-nine months (Jones, Barrack, and Skedros 2001). Springer et al. followed sixty-nine knees for an average of six years and similarly found patellar complications were the most common mechanical complication of a kinematic rotating hinge prosthesis (Springer et al. 2001).
Algorithm
Exposure is often limited in complex and revision TKA due to arthrofibrosis and capsular contractures. A median parapatellar approach is traditionally used. Continue with a thorough synovectomy medially and laterally and attempt to mobilize and evert the patella. Contractures of the extensor mechanism can be solved using a quadriceps snip, tibial tubercle osteotomy, or V-Y turndown. An episiotomy of the articular side scar tissue at the level of the patellar tendon is performed, gently going deeper towards the tendon with electrocautery until fat can be observed. Once the fat pad is found, the remaining scar tissue can be removed to the level of the fat pad. At this stage, the patella is usually capable of being everted.
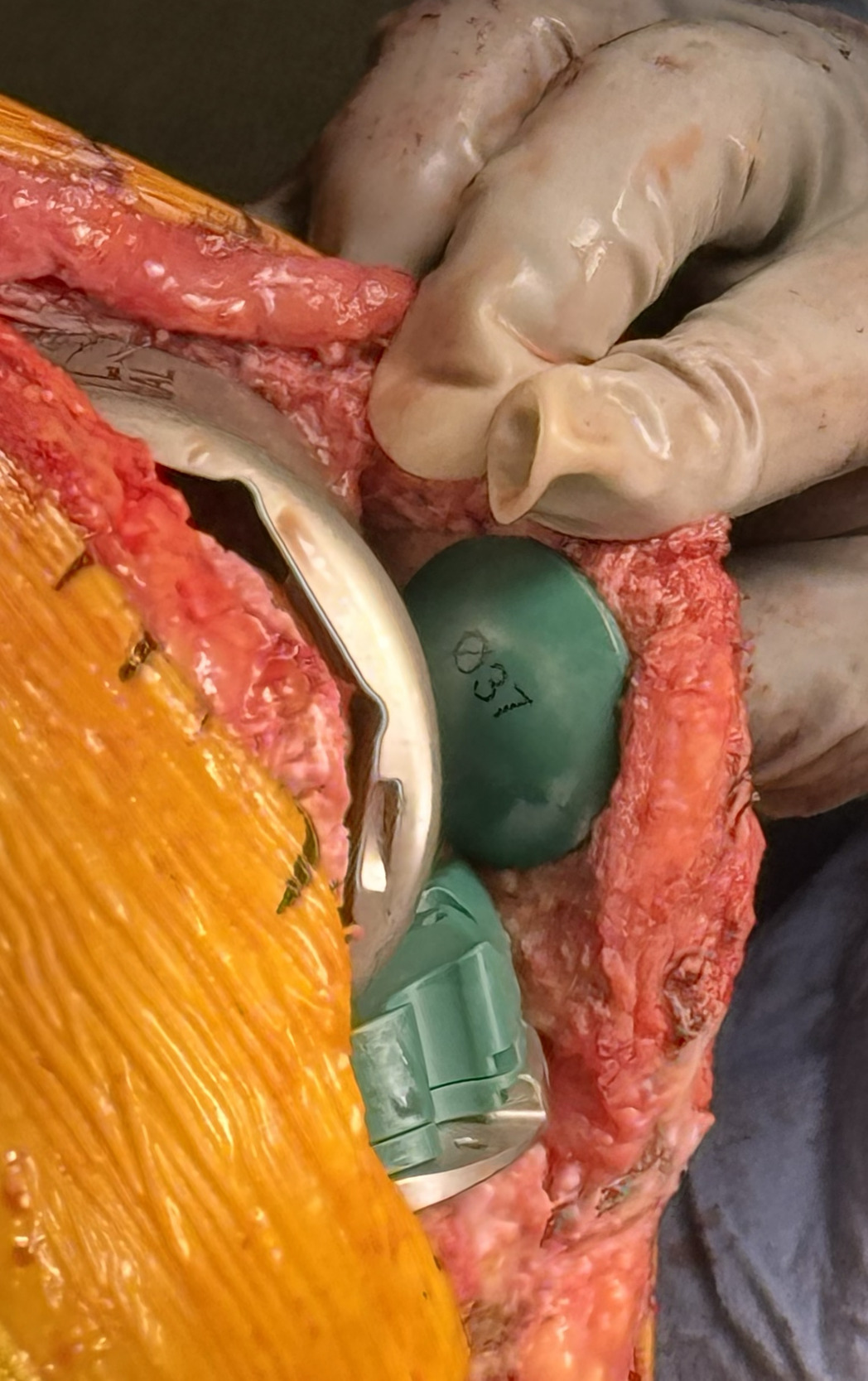
Once exposure has been achieved, components should be removed by surgeon preference. Bone edges of the femur and tibia should be refined and recut without concern for the joint line at this time. Trials should be done using a CCK with the largest size femoral component from medial to lateral and placed as posterior as possible without notching. This closes down the flexion space in the AP dimension.
Once both components are placed add the polyethylene ONLY evaluating flexion. Continue increasing the thickness of the polyethylene liner until flexion is balanced no matter how thick of a liner is required. Then, and only then, the knee is brought into extension. If extension is too loose, distal augments are added to the femur. If extension is too tight, greater distal femur resection is necessary; although, this is rare in complex and revision TKAs. Once balance in extension is achieved, evaluate the patella for maltracking and patella baja. The presence of patella baja at this balanced stage means the joint line must be distalized and the only way to bring the joint line down is to loosen flexion indicating one must convert to a rotating hinge.
Fundamentally, if a CCK trial is unable to be balanced in flexion or a Baja is created to obtain stable flexion space then conversion to a rotating hinge is necessary. With modern biological fixation methods this surgeon now believes the old dogma that bone stock dictates the need for a Hinge prosthesis is outdated and all surgeons should understand that MCL stability in flexion is the determining factor. There is validity that enough bone may be lost but with that the MCL by definition will incompetent and therefore the hinge is required.
In this clinical opinion article, this surgeon emphasizes three principles when implanting a rotating hinge.
“Nevins 3 Golden Rules”
-
A rotating hinge only requires extension balancing
-
Patella baja must be avoided
-
Place the implant in external rotation to reduce patellar complications
Conclusion
Rotating hinges have found greater popularity in complex and revision TKAs as an implant with maximum constraint in the case of severe bone loss. However, the exact indications to convert a CCK to a rotating hinge should be determined by the presence of patella baja after increasing polyethylene thickness to achieve balance in flexion. Future research should be directed at long term outcomes from CCK conversion to rotating hinge in various clinical settings.