Introduction
While multiple graft options exist for anterior cruciate ligament reconstruction (ACLR), bone-patellar tendon-bone (BPTB) autografts have historically been the gold standard (Fu and Schulte 1996). Advantages of BPTB include reproducible osseous integration through direct bone-to-bone contact, robust fixation, decreased risk of tunnel dilation, and favorable clinical and functional outcomes (Masuda, Taketomi, Inui, et al. 2018; Suzuki, Shino, Nakagawa, et al. 2011). Additionally, BPTB has been shown to have higher rates of return to sport compared to hamstring tendon autografts (DeFazio, Curry, Gustin, et al. 2020; Rahardja et al. 2021).
However, a unique surgical challenge in arthroscopic ACLR with BPTB is graft-tunnel mismatch (Boddu et al. 2015; Brown, Brophy, Franco, et al. 2007; Denti, Bigoni, Randelli, et al., n.d.; Graf, Dart, MacLean, et al. 2023; Ko et al. 2018). Inaccurate measurement of the femoral and/or tibial tunnels as well as a longer graft can lead to bone plug recession into or protrusion from the femoral or tibial tunnel (Boddu et al. 2015; Brown, Brophy, Franco, et al. 2007; Graf, Dart, MacLean, et al. 2023; Ko et al. 2018). Graft mismatch can ultimately lead to inadequate graft fixation and potential graft laxity, predisposing the patient to graft failure (Ko et al. 2018). Graft tunnel mismatch in arthroscopic ACLR has been reported in the literature at a rate between 13% and 26% (Nawabi, van der List, and Williams 2017; Shaffer, Gow, and Tibone 1993; Verma et al. 2005). While not all mismatches result in poor clinical outcomes for the patient, limiting graft tunnel mismatch is still of interest (Boddu et al. 2015; Brown, Brophy, Franco, et al. 2007; Graf, Dart, MacLean, et al. 2023; Ko et al. 2018; Shaffer, Gow, and Tibone 1993; Golish et al. 2007; Hensler et al. 2013; Miller and Hinkin 1996). One method of reducing graft-tunnel mismatch is advancing the graft bone plug deeper into the femoral tunnel and burying interference screws into the bone plug (Shah, Heckman, and Gilley 2009). While this method may decrease bone plug extrusion into the joint space, a larger anterior defect is created on the femoral tunnel, which can cause notch impingement and inferior graft outcomes (Shah, Heckman, and Gilley 2009).
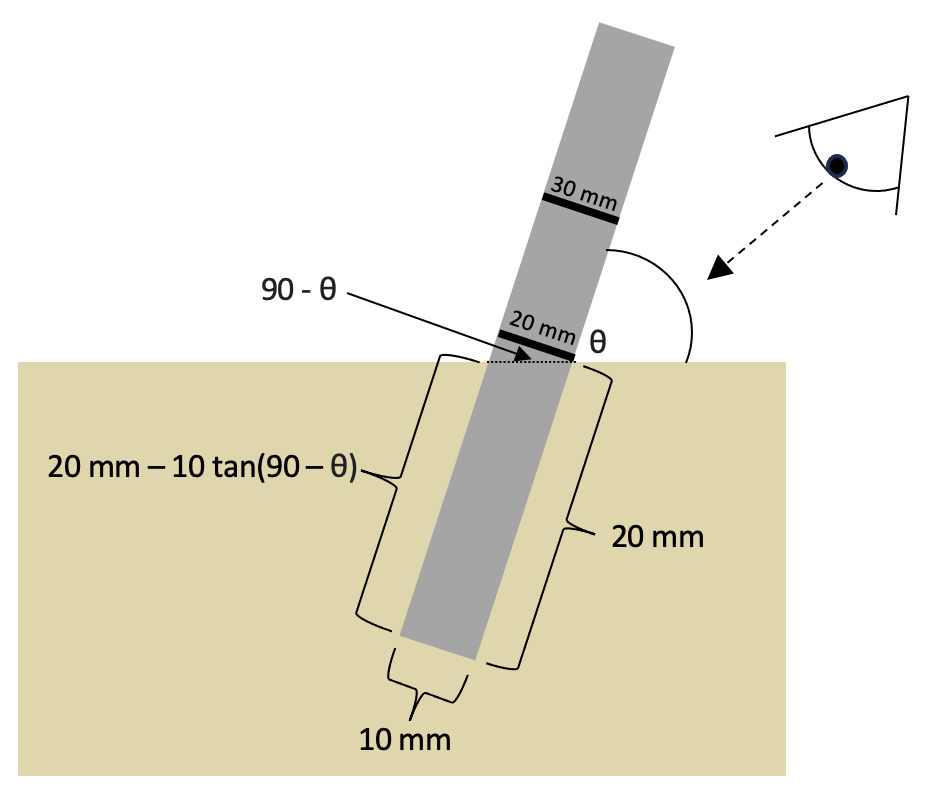
With arthroscopic surgical approaches, the tunnels are drilled with calibrated drill bits with depth markings printed on the perimeter. This provides the surgeon with an estimate of the depth of the tunnel without having to pass a second measuring device through the arthroscopic ports. We hypothesize that the calibrated drill bits may not consistently reflect the actual length of the tunnel when the tunnel is drilled at an oblique angle relative to the cortex of the bone, which may result in a shorter femoral tunnel length than what is measured by the calibrated drill bit.
The purpose of this study is to identify the difference in measured versus actual femoral tunnel depths with anteromedial, transtibial, and flexible drilling techniques. We hypothesize that the calibrated arthroscopic drill bit systematically underestimates the depth of the femoral tunnels. Understanding this difference can improve graft preparation and surgical technique in ACLR with BPTB.
Methods
Twelve fresh-frozen, midthigh-to-toe cadaveric legs were procured for this study. Cadaveric ages ranged from 69 to 93. Specimens included four male and five female knees, with two pairs consisting of a right and left knee from the same donor. The donors’ BMIs ranged from 17.03 to 24.27, with an average of 20.0. None of the knees had a prior history of trauma or knee surgery.
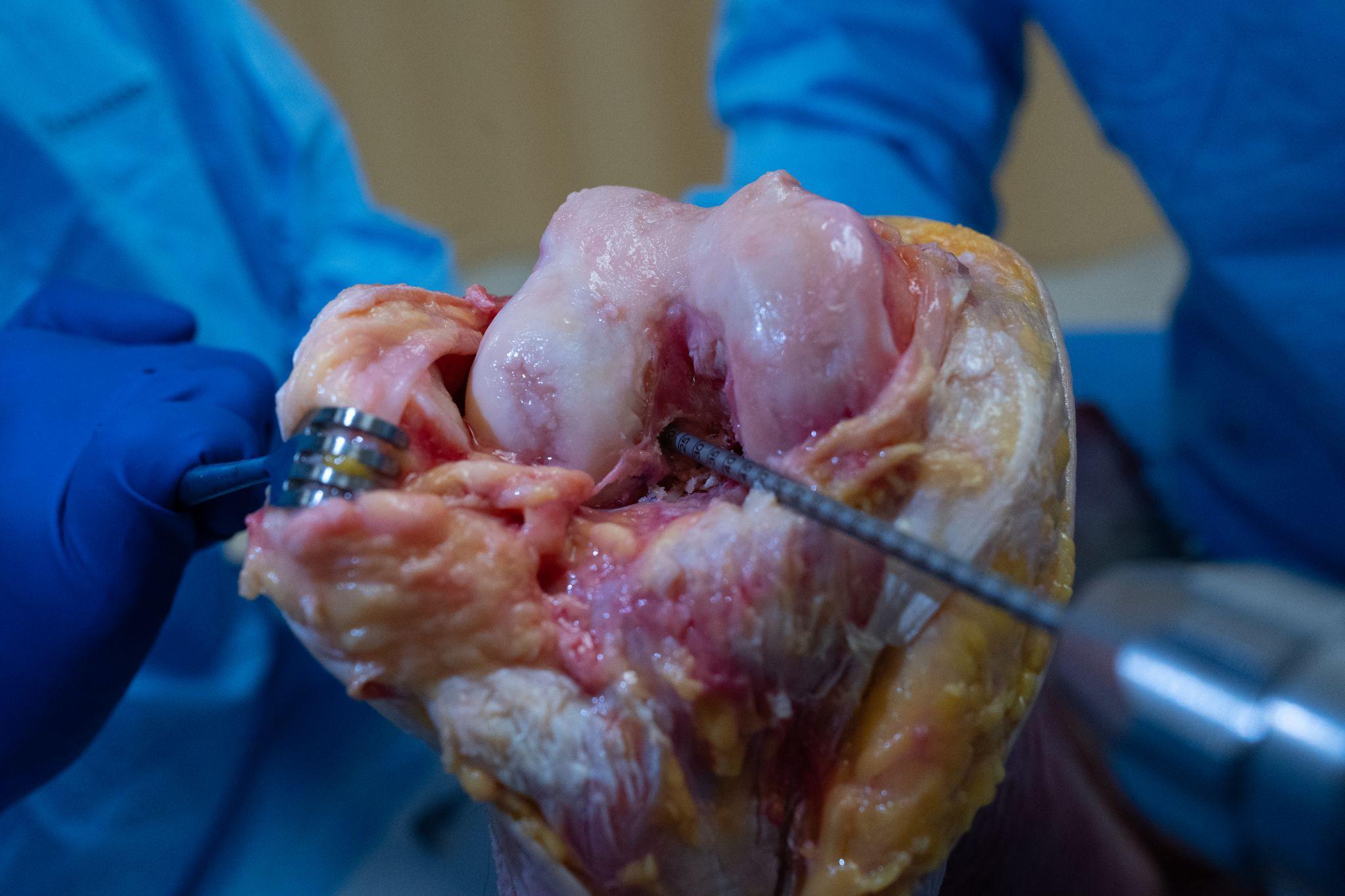
An open exposure through an extended medial parapatellar approach was performed to allow for high visualization and increased accuracy for correct femoral tunnel placement. With the knee flexed, a longitudinal incision was made, starting 5 cm above the superior pole of the patella and extending past the level of the tibial tubercle. Dissection was carried out between the vastus medialis and quadriceps tendon. A medial parapatellar arthrotomy was performed, and the infrapatellar fat pad was excised. The patella was dislocated and flipped laterally, allowing for complete joint visualization. The native ACL tendon was dissected and removed to prepare for the drilling of the bone tunnels and the native insertion site.
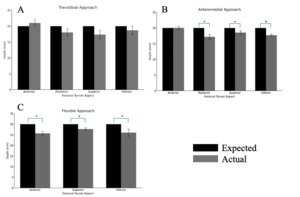
For all three femoral tunnel drilling techniques, bone tunnels were drilled using a 10mm diameter drill bit with millimeter depth markings. For all three techniques, the femoral tunnel was drilled to a depth of 20 mm, while the flexible approach tunnels were drilled to a depth of 30 mm to match the length of interference screws available during each procedure. As in an arthroscopic approach, the anterior aspect of the tunnel was utilized as the measured depth (knees flexed to 120 degrees with anteromedial drilling and 90 degrees for flexible and transtibial drilling) (Figure 1). After the tunnel was drilled (Figure 2), the anterior, posterior, superior, and inferior positions of the bone tunnel were measured using a depth gauge, as demonstrated in Figure 3. The posterior measurement was not able to me measured for the flexible approach given interference from the lateral femoral condyle. Measurement values were recorded to the nearest millimeter in correspondence to the calibration on the depth gauge. All measurements were made by a single senior orthopedic sports medicine surgeon.
Data analysis involved calculating the mean difference between the expected and actual tunnel depths for all aspects. The posterior aspect of the flexible approach was not measured because of the inability to place the depth gauge due to anatomical restrictions. The mean tunnel depths were then analyzed using a two-sample t-test. All statistical analyses were performed using SPSS version 27 (IBM, Armonk, NY, USA). A p < 0.05 was considered significant for all comparisons.
Results
Anteromedial drilling technique
For the anteromedial approach, the anterior aspect was used as a reference point for drilling the femoral tunnel, showing no difference in the expected and actual depths (20 mm, p = 1.00). The average posterior (17.2 mm, p < 0.05), superior (18.5 mm, p < 0.05), and inferior (17.7 mm, p < 0.05) aspects all showed a statistically significant decreased actual tunnel depth compared to the predicted depth (Figure 1, Table 1).
Transtibial drilling technique
The transtibial approach showed no significant differences between the expected and actual depts for all aspects of the femoral tunnels. Similar to the anteromedial approach, the anterior aspect was used as a reference point for drilling the tunnel with an average depth of 21.0 mm (p = 0.34), the posterior aspect had an average depth of 18.0 mm (p = 0.16), the superior aspect had an average depth of 17.3 mm (p = 0.12), and the inferior aspect had an average depth of 18.7 mm (p =0.37) (Figure 1, Table 1). None of these measurements were statistically significant from the expected depth of 20 mm.
Flexible drilling technique
The flexible approach showed statistically significantly shorter tunnel depths in the anterior (25.7 mm, p < 0.05), superior (27.7 mm, p < 0.05), and inferior (26.0 mm, p < 0.05) aspects compared to the expected depth (Figure 1, Table 1). Due to physical constraints with the medial femoral condyle, the depth gauge could not be passed to measure the posterior aspect and was thus excluded from the analysis.
Discussion
The current study demonstrated that the transtibial showed the lowest variability between the expected and actual femoral tunnel depths while the anteromedial and flexible approaches showed statistically significant differences in the expected and actual femoral tunnel depths in all three out of the four anatomic aspects (Figure 4, Table 1). In all drilling techniques, the superior, inferior, and posterior positions showed a shorter-than-expected femoral tunnel. This demonstrates an inherent difference between the measured tunnel depth based on the drill bit markings and the actual tunnel depth.
Our results demonstrate that the surgical approach and angle at which the tunnel is drilled is a major contributor to the difference in measured and actual tunnel lengths. Due to the anatomy of the femoral condyles and the placement of the femoral tunnel in an anatomic position, the drill bit must be inserted at an oblique angle relative to the cortex of the bone (Figures 2 and 5). This oblique angle causes an underestimation of the posterior and superior position, through the relationship shown in Figure 5, with the difference being a factor of both the drill bit diameter and approach angle. The transtibial approach drills a femoral tunnel at an angle closer to the perpendicular compared to the anteromedial approach, which may explain the decreased variance of the transtibial approach.
While the flexible reamer allows for a more perpendicular entry into the bone at the anatomic position of the femoral tunnel, which should decrease the variability in expected and actual lengths based on the relationship explained in Figure 5, we observed that the actual tunnel depths were significantly shorter than expected (Taneja, Jaiman, and Chopra 2021). One explanation for this may be that the flexible approach drills on a curvilinear path while the anteromedial and transtibial create straight tunnels. The depth gauge used to measure the tunnels also uses a straight and rigid probe to measure the depth, and measuring a curved path with a straight line would similarly underreport the actual length. While this may not affect soft tissue graft passage, it may affect measurements based on the fixation device used. When utilizing a bone plug, this may “bottom out” prematurely, given the fixed length of the bone plug. Ideally, a bone plug placed flush on the cortex after graft passage allows true aperture fixation and minimizes trauma to the graft during screw fixation and post-operative period by reducing repetitive lateral movement of the graft, commonly referred to as the “windshield-wiper” or “bungee cord” effect (Yang et al. 2003). In contrast, overestimating the tunnel length can force surgeons to place the tibial interference screw inaccurately, leading to articular penetration, screw divergence, or graft laceration (Olszewski, Miller, and Ritchie 1998).
Graft tunnel mismatch is well-known in the literature, and multiple techniques have been suggested to counteract the tendency of femoral tunnels being shorter than indicated by the calibrated drill bits. Golish et al. found that placement of the femoral tunnel within different locations on the lateral femoral condyle affects the maximum depth of the tunnel (Golish et al. 2007). Some positions, especially more horizontal placement from medial portal and far medial tibial tunnel approaches, constrained the femoral tunnel to be shorter than 2 cm to limit the risk of perforating the opposite cortex (Golish et al. 2007). For surgeons working in these conditions, corrective overestimation increases variability and could lead to weakening or violation of the femoral tunnel (Hammond et al. 2011; Mitchell et al. 2016). To optimize anatomic tunnel placement and maximize depth, Golish et al. recommended the transtibial tunnel technique, which is in agreement with our findings of the transtibial approach having the most reliable tunnel measurements (Golish et al. 2007; Jennings et al. 2017; Manderle, Beletsky, Gorodischer, et al. 2021).
Although our study found that the transtibial technique conferred the greatest accuracy, it comes with tradeoffs. Giron et al. concluded that truly anatomic femoral tunnel origin could not be reliably achieved through the transtibial technique (Giron et al. 2007). To this end, some surgeons may prefer the anteromedial approach to allow the femoral tunnel to be drilled independently of the tibial tunnel, while others may even opt for the double-bundle approach, which allows for increased anatomic placement of the anteromedial bundle and the posterolateral bundle of the graft though the use of two separate femoral tunnels (Giron et al. 2007; Teng, Cai, Wang, et al. 2024). Orthopedic surgeons should be aware of these variations in approaches and take steps to adjust and correct for such differences intraoperatively. However, further studies are needed to precisely measure drill bit angles and account for patient-specific anatomic variations to give more precise recommendations for surgeons on how to accurately and reliably adjust for differences in expected and actual femoral tunnel depths.
Our study does have limitations. First, the sample size is small, affecting the power of the study. While the femoral tunnels were measured in a fashion similar to what could be expected in an operating room, other techniques, such as CT measurements, could obtain more precise results. Additionally, our study used an open medial parapatellar approach to allow for more consistent femoral tunnel footprint placement. However, most ACLR surgeries are performed arthroscopically, which may slightly alter the angle of drill insertion, although we expect this difference to be minimal. Finally, the accuracy of the depth gauge is another limitation of the study. Future studies may be able to more precisely measure tunnel depths with advanced imaging and software.
Conclusion
This study quantitatively demonstrated that femoral tunnels are statistically significantly shorter for anteromedial and flexible approaches compared to the desired depth. The transtibial approach demonstrated shorter than expected tunnels, but this was not statistically significant. Our results suggest that femoral tunnels drilled through a transtibial approach may be the most accurate.