The OrthoBiologic Institute
Steven Sampson, DO
I would like to officially welcome you all to the first-ever TOBI Virtual Conference. We are super excited about this event and we understand this has been a really difficult time for the worldwide community of clinicians out there. Given that thought should we continue TOBI after we realized we could not do this in Las Vegas and be together, we felt the need to press on.
For the last eleven years, TOBI has really stood for a place where the community can gather and innovate and create a group effort and community together. And so, we really felt important to press on and I hope you really enjoy this experience that we are going to be delivering for you.
So, when thinking about Orthobiologics, I was looking at the past four decades in terms of how far we have come yet we are still in our infancy. And so when we see here, we typically began around the mid-'80s with Philippe Hernigou with the concept of the rationale for cell therapies for osteonecrosis of the femoral head. Then shortly afterward through cardiothoracic surgery with Dr. Ferrari, we learned more about PRP application. And then at the end of the 80s decade, we had the first patient treated for osteonecrosis of the femoral head by Dr. Hernigou.
In 1991, Arnold Caplan coined the term MSC’s. And then hyaluronic acid came on to the marketplace, followed by a maxillofacial surgeon [inaudible] and Mark, sharing their work with PRP. Ellen Mishra published a small pilot study on the American Journal of Sports Medicine on PRP, followed by Chris Santino explaining the rationale for bone marrow concentrate in the hip.
I personally published a review article of PRP at the time in 2008, which was then followed by the sensation in the media of a Super Bowl athlete, Hines Ward receiving PRP, which really helped raise awareness, although with the lack of data at the time.
Then we had our first TOBI conference in 2010, followed by a level one multicenter trial with many of our colleagues on lateral epicondylitis. We have seen through that time lots of level one studies for knee osteoarthritis as well as for plantar fasciitis that we are going to hear about.
So, when we look at the next decade ahead, the next ten years, what are we looking at? And so, what has COVID taught us? And for most of us, these last three months have really given us a rare time to take pause and look at our practice model. How we are treating patients? How we are running our practice? What is working? What is not working? It really exploited a lot of holes in the Healthcare System where there is a lack of access and communication around the world and how we can best help patients. We are innovators. The TOBI community is poised to pivot in thrive in this situation. We have always been pushing the envelope and not accepting the status quo of standard corticosteroid injections and temporary relief. So we are poised to pivot and thrive.
So what our goal should be? The theme of inclusivity. Societies are going to hear a lot about this weekend. They are all marching with the same singular voice. Physicians and industry, we all need to work together to advance this field and promote the credibility that we deserve.
We need a seat at the table with the government in the FDA. We need to advocate. All too often clinicians are not being included at the table and our voices are not being heard. As a group, we need some clarity on which biologics we can and cannot use so we stay within the speed limit and you will be hearing about some of that this week. We need more level one control trials. We need to be integrating massive clinical data. The technologies here, most of us in standard clinical practice can now integrate data registry and collection of outcomes.
You are going to be hearing about classifications, cell counting and really standardizing our biologics so we know what we are putting in our patients and what is working and what is not. And lastly, we are going to be getting more tools from the industry so that we can potentially help our patients.
Our ultimate goal here, the big picture ten thousand foot view, as a global community, is widespread patient access to Orthobiologics. We have almost a thousand practitioners and attendees tuning in from around the world and are starting to spread the reach of these biologics. We need to overcome the challenges and continued widespread use and access not to a select few but to the global community.
I want to thank our faculty as well as our sponsors. Without our sponsors, we could not put on such a production, as well as our faculty. I know it is very challenging and awkward doing a Zoom based lecture and live. In many cases, it can be quite difficult. We appreciate you taking time away from your family as we are getting back to practice and really emphasizing the importance of doing this together. In honor of our faculty, we have donated to the San Diego Foundation, which is a non-profit dedicating research a hundred percent towards COVID using cell therapies.
So, I really hope you enjoy the show. It should be really interesting and something that has really never been done before and we thought why not?
Introduction to The ON Foundation
Brian Cole, MD
I am Dr. Brian Cole from Rush University Medical Center in Chicago. I want to congratulate Dr. Samson for his nimbleness in continuing to proceed with his meeting in a virtual way. I commend you, I know this is a challenging time and I know how much time and effort you put into developing a meeting of this caliber. Sorry, we cannot be there in person, but I wish you the best and I wish the audience and the participants have a terrific educational experience. I would not expect anything less.
I am speaking just for a couple minutes on behalf of the ON Foundation. This is an organization that I have been involved with for approximately four years, and the vision of the ON Foundation is, basically, to provide a network that is independent, whose promises to evaluate and provide research, support, and educational initiatives and auto regeneration. It is an international foundation and it is as an emphasis in driving the field of Orthopedic Tissue Regeneration and driving the development and understanding of new treatment strategies for the well-being of the patient, much likely the initiative and vision of the TOBI Conference. To emphasize, we drive innovation, we improve clinical practice, we foster our network and our goals are to help the patients.
Clearly collaboration is key. We have learned through our collaborative initiatives that that is the core of our success. We collaborate with academic societies. They follow similar goals and share our vision. The collaborations are very flexible and includes a support for an investigator, shared educational programs and co-organization of scientific events and much more. We currently partner with the number of societies including the AAOS, ANA, the AGA, AOSM, URS, Euro Spine, ICRS, the ICRS, the ORS, all with the promise of advancing auto regeneration.
The nature of these collaborations primarily, as it relates to TOBI now is on educational grants and grantees are getting a financial contribution to attend or participate in this educational event. Scholarships are providing their contribution to attend educational events, fellowship programs where we can allow individuals who are interested to visit one of several research centers, either focusing on clinical or basic science research and again with the emphasis on auto regeneration. A number of awards for investigators and clinician scientist, who make major contributions in the field of auto regeneration, and a number of innovation grants such as our literature grants, Kickstarter grants, pilot grants and break through grants.
I would ask that you take a minute while you are attending the Virtual TOBI Conference and sign up for the ON Foundation. It will keep you apprised for all the on goings. It is a community platform that will connect scientists and practitioners worldwide and provide information tools if there is no sign-up fee. It is purely for informational purposes and primarily it allows you to get access to these educational initiatives and collaborations that I have outlined, including funding for a variety of meetings and scholarships. So, if you are interested, maybe you could just take a minute and sign up on www.on-foundation.org. This is where you can register and, in the future, received latest information and get access to the educational research support, and also connect with one another who are like-minded in the consideration for auto regeneration.
If you would like to learn more before signing up, certainly go to the on-foundation.org website, it is on-foundation.org. And please follow us on our social media links. Thank you, and I wish you the best in attending the International TOBI Conference this year.
Consensus Statement on Minimal Reporting Requirements & Classification of PRP
Gerard Malanga, MD
New Jersey Sports Medicine, Cedar Knolls, NJ
Kon Elizaveta, Di Matteo Berardo, Delgado Diego, Cole Brian J, Dorotei Andrea, Dragoo Jason L, Filardo Giuseppe, Fortier Lisa A, Giuffrida Alberto, Jo Chris H, Magalon Jeremy, Malanga Gerard A, Mishra Allan, Nakamura Norimasa, Rodeo Scott, Sampson Steve, Sánchez Mikel
Orthobiologic strategies can be considered a path to “personalized medicine” which has tremendous potential for improved treatments of orthopedic conditions. We have an abundance of clinical trials that used many different PRP products. Few of these studies are high quality, double-blinded RCTs. Multiple systematic reviews (perhaps more than high quality trials) and an interesting number of meta-analyses have been published. We analyzed the outcomes of all the available meta-analyses evaluating intra-articular PRP injections in patients affected by knee or hip OA. A total of 48 articles were identified through databases searching. After title and abstract screening, 47 studies were included. Ultimately, a total of 13 studies published from 2013 to 2020 were included, dealing with the comparison of intra-articular PRP injection to intra-articular HA, CS, or placebo for the treatment of hip or knee OA. Twelve meta-analyses on knee OA, and one on hip OA were included, with a number of patients ranging from 303 to 1,543. Patients with all grades of OA were included, with a majority of patients being affected by mild to moderate OA (Kellgren-Lawrence I-III and Ahlbäck 1-3). The majority of these studies and meta-analyses are flawed by the lack of consistent reporting of the PRP products used. Even with the limitations in reporting on the PRPs injected, the current literature supports the conclusion that PRP is superior to NS/corticosteroids/HA for mild to moderate knee OA.
A new coding system for PRP procedures is proposed by this expert group called the “Code System”. The code is a sequence of 6 digits grouped in pairs indicating parameters of platelet composition, purity and activation with specific definitions for each code: N1-N2-N3-N4-N5-N6. This new PRP classification and coding system could provide a step forward in this direction, fostering the further development of this promising biological approach for the treatment of OA and other musculoskeletal conditions.
Positive Effect of Platelet-Rich Plasma on Pain in Plantar Fasciitis: A Double-Blind Multicenter Randomized Controlled Trial
Taco Gosens, MD
Orthopaedic Surgeon Elisabeth Tweesteden Hospital Tilburg, NETHERLANDS
Joost C. Peerbooms, Paul Lodder, Brenda L. den Oudsten, Kamiel Doorgeest, Hans M. Schuller and Taco Gosens
Background: When nonoperative treatment for chronic plantar fasciitis fails, often a corticosteroid injection is given. Corticosteroid injection gives temporary pain reduction but no healing. Platelet-rich plasma (PRP) has proven to be a safe therapeutic option in the treatment of tendon, muscle, bone, and cartilage injuries.
Purpose: To determine the effectiveness of PRP as compared with corticosteroid injections for chronic plantar fasciitis.
Study Design: Randomized controlled trial; Level of evidence, 1.
Methods: Patients with chronic plantar fasciitis were allocated to have steroid injection or PRP. The primary outcome measure was the Foot Function Index (FFI) Pain score. Secondary outcome measures were function, as scored by the FFI Activity, FFI Disability, and American Orthopaedic Foot & Ankle Society, and quality of life, as scored with the short version of the World Health Organization Quality of Life (WHOQOL-BREF). All outcomes were measured at baseline and at 4, 12, and 26 weeks and 1 year after the procedure.
Results: Of the 115 patients, 63 were allocated to the PRP group, of which 46 (73%) completed the study, and 52 were allocated to the control group (corticosteroid injection), of which 36 (69%) completed the study. In the control group, FFI Pain scores decreased quickly and then remained stable during follow-up. In the PRP group, FFI Pain reduction was more modest but reached a lower point after 12 months than the control group. After adjusting for baseline differences, the PRP group showed significantly lower pain scores at the 1-year follow-up than the control group (mean difference, 14.4; 95% CI, 3.2-25.6). The number of patients with at least 25% improvement (FFI Pain score) between baseline and 12-month follow-up differed significantly between the groups. Of the 46 patients in the PRP group, 39 (84.4%) improved at least 25%, while only 20 (55.6%) of the 36 in the control group showed such an improvement (P =.003). The PRP group showed significantly lower FFI Disability scores than the control group (mean difference, 12.0; 95% CI, 2.3-21.6).
Conclusion: Treatment of patients with chronic plantar fasciitis with PRP seems to reduce pain and increase function more as compared with the effect of corticosteroid injection.
Registration: NCT00758641 (ClinicalTrials.gov identifier).
Keywords: orthobiologics; platelet-rich plasma; musculoskeletal; regenerative medicine
Delaying Need for Knee Arthroplasty with PRP Injections
Diego Delgado, PhD
Advanced Biological Therapy Unit, Arthroscopic Surgery Unit, Hospital Vithas Vitoria, Vitoria-Gasteiz, Spain
Knee osteoarthritis (KOA) is a degenerative disease with a high prevalence and impact worldwide. Current treatments do not modify the disease and focus on symptom relief, being total knee arthroplasty the ultimate solution for these patients. It implies a high cost for the healthcare systems and potential future complications. The biological action of Platelet-Rich Plasma (PRP)3 and other biological treatments could slow down the disease progression, resulting in remarkable delay in joint replacement. A retrospective study and a survival study were conducted to address this issue. The former analyzed KOA patients who underwent total knee arthroplasty and had previously received PRP infiltrations. The second evaluated patients who received PRP infiltrations with a 5-year follow-up in order to know if they had to undergo surgical intervention. This work included more than 1000 patients and it showed a delay in knee replacement of more than 5 years. In addition, more than 85% of patients who began PRP treatment did not undergo total knee arthroplasty at a 5-year follow-up. The severity degree, age, PRP cycles and the administration route significantly influenced the efficacy of PRP in delaying surgery. Therefore, PRP application may delay the placement of the knee arthroplasty in KOA patients.
Single Injection of Leukocyte Rich PRP vs BMC for the Treatment of Knee OA: 1 Year Results
Joshua G. Hackel, MD Andrews Institute, Gulf Breeze, FL
Abstract
Purpose: To compare the efficacy of BMC to PRP on pain and function in patients with knee osteoarthritis up to 24 months after injection. It was hypothesized that patients receiving BMC would have better outcomes over time than those receiving leukocyte-rich PRP.
Methods: A total of 90 participants aged between 18 and 80 years with symptomatic knee OA (Kellgren-Lawrence (KL) grades 1-3) were randomized into 2 study groups: PRP and BMC. Both groups completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and subjective International Knee Documentation Committee (IKDC) questionnaires before and 1, 3, 6, 9, 12, 18, and 24 months after a single intra-articular injection of leukocyte-rich PRP or BMC.
Results: 84 patients completed questionnaires from baseline to 12 months, however 11 patients (n=7 PRP group) were lost to follow-up at 18 months and 19 (n=11 PRP group) were lost at 24 months. No differences in IKDC (p=0.909; 95%CI: -6.3,7.0) or WOMAC (p=0.789; 95%CI: -6.3,4.8) scores, over time, between the groups were observed. Both groups had significantly improved IKDC (p<0.001; 95%CI: 0.3,0.6) and WOMAC (p=0.001; 95%CI: -0.4,-0.1) scores from baseline to 24 months after the injection. These improvements plateaued at 3 months and were sustained for 24 months after the injection.
Conclusions: Both PRP and BMC were effective in improving pain and function in patients with knee OA for at least 24 months. This study did not prove BMC to be superior to PRP.
Level 1 Evidence: Double-blind, Randomized Clinical Trial Comparing PRP vs Corticoids for Rotator Cuff
Victor Vaquerizo, MD
Príncipe de Asturias University Hospital, Alcalá de Henares, Madrid, Spain
Rotator cuff tendinopathy (RCT) is a painful and dysfunctional shoulder condition where immunocompetent cells and activated stromal fibroblasts lead to a non-resolved inflammatory condition. The aim of this study was to compare the clinical efficacy of intratendinous injections of plasma rich in growth factor (PRGF) with the conventional intratendinous corticosteroid injections on patients with rotator cuff tendinopathy using UCLA scale, QuickDash, and Constant test as shoulder pain and function outcome measures. Within the context of a single-center, prospective, randomized controlled clinical trial, patients received 3 infiltrations, one every other week of either PRGF (n=39) or Celestone Cronodose®(n=40) as a control group. Patients were evaluated before treatment, and at 3, 6, and 12 months as the end of follow-up using UCLA scale, QuickDash, and Constant test.
Both PRGF and Celestone Cronodose® groups showed significant clinical improvement in the UCLA, QuickDash, and Constant scores at all time points of the study compared with baseline scores (p<0.05). However, the UCLA and QuickDash scores of PRGF group at 6 and 12 months turned out to be 22,2% and 21,2%, (p<0.0001 and p<0.0001), and 32,6% and 30,7% (p<0.005 and p<0.05) superior to the Celestone Cronodose® group thereby corroborating the primary outcome of this CT.
Keywords: Platelet-rich plasma, Sports medicine, rotator cuff tendinopathy. Inflammation, Corticosteroids
References
-
Van den Dolder PA, Ferreira PH, Refshauge KM. Effectiveness of soft tissue massage and exercise for the treatment of non-specific shoulder pain: a systematic review with meta-analysis. Br J Sports Med. 2014 Aug;48(16):1216-26.
-
Riley G. Tendinopathy–from basic science to treatment. Nat Clin Pract Rheumatol. 2008 Feb;4(2):82-9.
-
Dakin SG, Buckley CD, Al-Mossawi MH, Hedley R, Martinez FO, Wheway K, Watkins B, Carr AJ. Persistent stromal fibroblast activation is present in chronic tendinopathy. Arthritis Res Ther. 2017 Jan 25;19(1):16.
-
Gaujoux-Viala C, Dougados M, Gossec L. Efficacy and safety of steroid injections for shoulder and elbow tendonitis: a meta-analysis of randomised controlled trials. Ann Rheum Dis. 2009 Dec;68(12):1843-9.
-
Rha DW, Park GY, Kim YK, Kim MT, Lee SC. Comparison of the therapeutic effects of ultrasound-guided platelet-rich plasma injection and dry needling in rotator cuff disease: a randomized controlled trial. Clin Rehabil. 2013 Feb;27(2):113-22
Meniscus Treatment Protocol in the Professional Athlete
Ramon Cugat, MD, PhD
Garcia Cugat Foundation, Barcelona, Spain
Meniscal injuries are extremely common in the general and athletic population. Patient’s age, activity level, meniscal tissue quality, tear pattern and tear location are among most commonly involved factors to decide on conservative or surgical treatment. The management strategy when surgical treatment is recommended has switched from meniscectomy to meniscal-preserving techniques over the years. It is nowadays extensively accepted that surgeons have to make their best to repair the meniscus and try to preserve as much tissue as possible.1 This is because of the potential negative long-term impact on the articular cartilage when meniscal tissue is removed. However, in many cases of poor meniscal tissue quality and complex tear patterns, the achievement of a stable repair technique with high success rate is not possible with standard repair techniques or configurations. Regenerative medicine, based on signaling molecules,2 cells and scaffolds, play a very important role in restoring the meniscus. Platelet Rich Plasma treatment may be used in conservative treatment and as biological augmentation in meniscus surgery to enhance options for repair and replacement.3
References
-
Seil R, Becker R. Time for a paradigm change in meniscal repair: save the meniscus! KSSTA. 2016;24:1421-1423.
-
Kaminski R, Kulinski K, Kozar-Kaminska K, et al. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study Evaluating Meniscal Healing, Clinical Outcomes, and Safety in Patients Undergoing Meniscal Repair of Unstable, Complete Vertical Meniscal Tears (Bucket Handle) Augmented with Platelet-Rich Plasma. Biomed Res Int. 2018;2018:9315815.
-
Moran CJ, Busilacchi A, Lee CA, Athanasiou KA, Verdonk PC. Biological augmentation and tissue engineering approaches in meniscus surgery. Arthroscopy. 2015;31(5):944-955.
Quantification of Platelet Growth Factors and Red Blood Cells in Platelet Rich Plasma, Bone Marrow Aspirate and Concentrate
Peter A. Everts, Gulf Coast Biologics, Fort Myers FL. John Ferrell, ROSM, Rockville MD
Moises Irizarry-de Roman, No Merci Sports Medicine, Miami FL Rowan Paul, California Orthopedics, San Francisco CA
Glenn Flanagan II, Naples Regenerative Institute, Naples FL. Kenneth Mautner, Emory University GA
Synopsis of lecture
The application of biological therapies may offer solutions in musculoskeletal pathologies, spinal disorders, chronic wound care, and critical limb ischemia, to effectively change the local micro-environment in order to support in tissue healing and facilitate tissue regeneration.
Bone marrow aspiration procedures, and in particular the use of bone marrow mesenchymal stem cells (BM-MSCs) are one of the key interventions when using autologous biological bone marrow cells for regenerative medicine clinical applications. The use of bone marrow aspirate (BMA) and bone marrow concentrates (BMC) is based on the fact that bone marrow cells, including their progenitor cells, nucleated cells, platelets, and other cytokines support in tissue healing and tissue regenerative processes. The primary focus has been the ability of MSCs to self-renew and differentiate into multiple cell types. Whereas the MSC immunomodulatory effects, and thus the roles of specific growth factors and trophic factors, have been rarely mentioned.
An effective BM-MSC injection is reliant on the performance of the marrow aspiration procedure: minimizing cellular trauma, while maximizing cellular yields, and simultaneously avoiding peripheral red blood cell (RBC) infiltration. BM aspiration procedures, and not diagnostics, are routinely performed using dedicated BM kits for regenerative medicine applications. Kits may include a harvesting needle system and/or BM concentration device. Various bone marrow needle harvesting systems are available on the market, each with their own proprietary design characteristics, and thus marrow aspiration dynamics when transferring marrow cavity cells through a needle system into collection syringes. Potentially, different needle design features might affect the quality and viability of harvested BM tissue, as well as the cellular yields. Therefore, BM needle system features and harvesting dynamics are important considerations when considering BMA procedures.
The literature pronounces BMAs as a heterogenous mix of cells, referring in most instances to MSCs, HSCs, and mono nuclear cells. Platelets, megakaryocytes, and RBCs are seldomly mentioned, let be subject to BM research. Physicians have been using a variety of harvesting needles during the last decades, including the traditional Jamshidi™ harvesting needle (Ranfac Corporation, Avon MA, USA). Based on design differences, not every BMA is born equal and cellular yields, composition, and viability might by very different among harvesting devices. For interpretation purposes, some of the cellular difference between two newly developed BMA needle harvesting systems, the Aspire Bone Marrow Harvesting System™ and the Marrow Cellution Bone Marrow Aspiration Device™ (EmCyte Corporation, Fort Myers FL, USA and Ranfac
Corporation, Avon MA, USA, respectively). A significant difference between the two harvesting systems is that the Marrow Cellution device is developed and used by physicians for low volume BMA aspiration only, followed by direct injection without filtration or processing. Therefore, these specimens mimic the marrow cavity cellular content and their specific cell concentrations. This includes a RBC content and hematocrit which is similar to the peripheral blood values. Conditional of the negative forces that occur with syringe pull during marrow aspiration, this particular BMA injectate can have high plasma free hemoglobin concentrations, which cannot be removed from the injectate. The Aspire™ harvesting system is designed to penetrate the trabecular bone, maintaining a quiescent tissue environment during deployment and collection, contributing to a reduction in tissue activation, plasma free hemoglobin content, and clotting. The Aspire™ harvesting system is intended to provide a BMA for centrifugation processing, leading in this occasion to the creation of Pure-SupraPhysiologic BMC® (EmCyte Corporation, Fort Myers FL, USA).
At four US institutions, 12 patients consented to a bi-lateral BMA harvesting model prior to their BM-MSC regenerative injection therapy for MSK disorders. Comparative laboratory data between the above-mentioned needle systems will be presented. Apart from comparing bone marrow only aspiration data, the effect of BMA centrifugation on cell concentrations is depicted to exemplify significant bone marrow cellular injectate differences between any BMA injectate, and a BMC vial, being the superior treatment biologic, with regard to total deliverable of stem cells, platelet count, hematocrit levels, trauma, and growth factor levels.
Bone Marrow Concentrate (BMC) 5 Year Outcomes Data
M&M: P. Acnes Septic Joint Following BMC/PRP for Shoulder Osteoarthritis
Kristin Oliver, MD
Regenerative Orthopedics Specialist & Sports Medicine Blue Tail Medical Group, Chesterfield, MO
Knee osteoarthritis is a leading cause of pain and disability worldwide. Non-surgical treatment options are limited. The potential for cellular based regenerative therapies to bridge the gap between short-term symptomatic relief and total knee arthroplasty has received abundant attention. This presentation includes pain and functional outcomes data on 1450 patients with knee osteoarthritis treated with intra-articular bone marrow concentrate. 52 of these patients are out 5 years from the date of treatment.
Treatment registry data for 1450 patients diagnosed with Kellgren-Lawrence Stage 2-4 knee osteoarthritis were analyzed. Data regarding adverse events, Visual Analog Pain Scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index metrics (WOMAC) were obtained at intervals up to 5 years.
Adverse events were limited to transient pain and swelling of the treated joint. The mean reported WOMAC changes from pre-procedure to two years post-procedure were as follows: Pain + 24, Stiffness +25 and Function + 20. The mean reported VAS was reduced from 4.7 at baseline to 2.3 at five years.
This study of intra-articular autologous bone marrow concentrate in patients diagnosed with knee osteoarthritis demonstrates encouraging results for positive outcomes without complication.
Bone Marrow-Derived Plasma: Undervalued Role in Orthobiologics
Ryan Dregalla, MD
Napa Medical Research Foundation, Napa, CA
The most commonly used autologous orthobiologics include bone marrow aspirate concentrate (BMAC), platelet-rich plasma(s) (PRP) and processed adipose tissue, especially with respect to osteoarthritis1. Historically, adipose and bone marrow-based therapies have been used for their mesenchymal stem/stromal cell (MSC) composition and PRP as a source of growth factors. However, recent work has illuminated the clinical value of MSC-associated secretomes2. Recently, Cassano, et al compared several soluble factors derived from freshly processed BMAC and PRP and found that interleukin receptor antagonist, an important immunomodulatory protein, was substantially higher in BMAC compared to PRP3. Intrigued by this finding, we sought to determine if platelets derived from peripheral and bone-marrow plasma showed distinct differences in soluble proteins following degranulation. To investigate this possibility, an array of growth factors, pro- and anti-inflammatory proteins were quantitated over an extended time course and normalized to the respective cell counts. Our findings begin to characterize the differences in platelets derived from the two plasma sources and provides a rationale for investigating the clinical use of bone marrow plasma as a therapeutic agent.
References
-
Sherman, B. J., Chahla, J., Glowney, J. & Frank, R. M. The Role of Orthobiologics in the Management of Osteoarthritis and Focal Cartilage Defects. Orthopedics 42, 66-73, doi:10.3928/01477447-20190225-02 (2019).
-
Harrell, C. R. et al. Molecular Mechanisms Responsible for Therapeutic Potential of Mesenchymal Stem Cell-Derived Secretome. Cells 8, doi:10.3390/cells8050467 (2019).
-
Cassano, J. M. et al. Bone marrow concentrate and platelet-rich plasma differ in cell distribution and interleukin 1 receptor antagonist protein concentration. Knee Surg Sports Traumatol Arthrosc 26, 333-342, doi:10.1007/s00167-016-3981-9 (2018).
DELPHI Consensus Panel: Recommendations on BMC to Treat Orthopedic Disease and Pain.
Christopher J. Centeno, MD Centeno-Schultz Clinic, Broomfield, CO
The field of interventional orthobiologics has little consensus on types of treatments or indications for same. The use of bone marrow concentrate is no exception. Hence, a Delphi panel of 25 private practice and academic physicians who use bone marrow concentrate in their day to day practice was convened. A list of questions was generated and approved by a steering committee and then sent to each participant with a 5 answer Likert scale indicating the degree of agreement or disagreement. The criteria for consensus of any statement was 80% agreement using the “Agree” or “Strongly Agree” choices. Deidentified aggregate answers for the group were shown to all participants between rounds who then considered the answers of their peers in subsequent rounds of voting. A total of 4 rounds was required to achieve agreement on 8 items of 11. These were the need to use a treatment registry, the use of candidacy grades, the need for expanded informed consent, the routine publication of research for new indications, the need for advertising grounded in science, using an IRB for new applications, and using imaging guidance for injection. Finally, the group came to consensus that the minimal level of research needed before clinical use of BMC was a case series to a comparison trial. Notably this group, that included many academics, did not agree that a randomized controlled trial was required before the use of BMC in orthopedic applications.
Intraarticular Microfat with and Without PRP for Knee Osteoarthritis: Completed Results
Jeremy Magalon, MD University of Aix-Marseille, Paris, France
INTRODUCTION : Osteoarthritis (OA) of the knee is one of the most frequent causes of pain, function loss, and walking-related disability among mature adults (>65 years) in the United States. MICROPREP is a prospective, single-center, comparative, open-label, phase II trial evaluating intra-articular Microfat – PRP injection in the OA of the knee
MATERIAL & METHOD: Ten milliliters of Microfat –mixed either with saline, PRP (1 billion platelets dose) or PRP (3 billion platelets dose) were injected into the knee joint under local anesthesia. The main endpoint was relaxation time using T2 mapping. Pain EVA, WOMAC and patient satisfaction were also evaluated up to 6 months of follow-up.
RESULTS : Thirty patients were randomized in three groups of ten patients and treated between December 2017 and January 2019. At 6 months follow-up, a significant change in pain of 34.0 ± 4.2 (p<0.0001) and improve function with mean change in WOMAC score of 20.7 ± 3.8 (p<0.0001) were observed. T2 mapping decrease in all groups at 6 months. No serious adverse events were identified during follow-up.
DISCUSSION: Microfat injection with PRP or not may be a promising product to alleviate pain and improve function in knee OA with a potential cartilage regeneration.
Effective Clinical Modulation of Knee OA Symptoms Through Combined Cellular Therapy (Lipoaspirate, BMC and PRP)
Dr. Kevin Darr, MD
Covington Orthopedic Sports Medicine Institute, Regenerative Medicine, Covington, CA
Vinet-Jones, Heather[1] PhD Candidate, and Darr, Kevin F[2] MD
Objective: The objective of this study is to assess the clinical outcome of participants receiving Combined Cellular Therapy (CCT), for the treatment of pain and functional deficits associated with osteoarthritis of the knee.
Design: All study participants received CCT of one or more knees to treat OA. The Harvest systems (TerumoBCT) were used to harvest and transfer autologous adipose tissue via suction lipoplasty, bone marrow aspirate concentrate (BMAC), and platelet rich plasma (PRP). At 6 weeks post CCT, PRP boosters were administered to patients who had not yet achieved 80% improvement in both scales.
Setting: Procedures were performed onsite in a fully equipped, sterile prepped procedure room.
Participants: 96 study subjects ages 38-90 with a clinical diagnosis of mild (n=34), moderate (n=58), and severe (n=48) OA of the knee with no other complicating clinical diagnosis who have completed follow ups at 6, 18, and 52 week intervals at a minimum.
Interventions: not applicable
Main Outcome Measures: Quantitative analysis of pain and function modalities were performed using the Visual Analog Scale (VAS) and the Knee Injury and Osteoarthritis Outcome (KOOS) Western Ontario and McMaster Universities Arthritis Index (WOMAC) respectively.
Level of Evidence: Level III evidence obtained from well-designed controlled trials without randomization.
Results: At the 6 and 18 weeks follow ups, all study participants reported significant improvement (p<0.001) from baseline in VAS and WOMAC in mild to severe knee OA cases, and also at yearly follow ups with mild and moderate OA. Severe OA had a return of some functional deficits as well as some return of pain but still significant improvement from baseline (p<0.001).
Conclusion: The use of CCT in mild to severe OA knee cases results in clinically significant improvement in both pain and functional scales, signifying cellular therapy as an orthopedic modality for the treatment of knee OA.
Keywords: Knee OA, Bone marrow aspirate concentrate (BMAC), PRP, Osteoarthritis; regenerative medicine
Randomized Crossover Clinical Trials: Adipose Injections for Plantar Fasciitis, Ball of Foot and Heel
Jeffrey Gusenoff, MD
Associate Professor of Plastic Surgery,University of Pittsburgh Medical Center,Pittsburgh, PA
Background: Plantar fasciitis is the most common cause of heel pain resulting from degeneration of the plantar fascia (PF). Current treatments are either invasive with complication risks, or non-invasive with inconsistent results.
Hypothesis/Purpose: To evaluate perforating fat injections on PF regeneration, pain and quality of life.
Study Design: Prospective, randomized, cross-over pilot study
Methods: Patients with PF thickening (>4mm) who failed standard treatment for 6 months or longer were included. Subjects were randomized to intervention/Group 1: perforating autologous fat injections to the PF or Group 2: observation. Group 1 was followed for a year, and Group 2 was observed for 6 months and crossed over to procedure with 6 months follow up. Results included: validated foot pain and quality of life questionnaires, PF thickness measured by ultrasound, and complications.
Results: Group 1 had 9 female subjects and Group 2 had 4 women and 1 man. At 6 and 12 months, Group 1 PF thickness decreased compared to baseline (p<0.05).
Group 2 had decreased PF thickness at 6 months post-injection (p<0.05). Group 1 had pain improvements at 6 and 12-months post-operative (p<0.01) compared to baseline. Group 2 reported no pain difference after injections. Group 1 improved activities of
daily living and sports activity at 6 and 12 months (p<0.003), Group 2 noted increased sports activity 6 months post-injection (p<0.03).
Conclusions: Perforating fat injections to the PF demonstrate promising improvements in pain and daily activities, as well as regenerative potential in remodeling thickened PF.
Clinical Relevance: Fat injections for chronic plantar fasciitis is a safe, novel, minimally invasive procedure that improves pain, quality of life, and restores the plantar fascia.
Combating COVID-19 with MSCs
Christopher Rogers, MD
San Diego Orthobiologics Medical Group, Carlsbad, CA
In late 2019, a novel coronavirus (SARS-CoV-2) emerged in Wuhan, capital city of Hubei province in China. Cases of SARS-CoV-2 infection quickly grew by several thousand per day. Less than 100 days later, the World Health Organization declared that the rapidly spreading viral outbreak had become a global pandemic. Coronavirus disease 2019 (COVID-19) is typically associated with fever and respiratory symptoms. It often progresses to severe respiratory distress and multi-organ failure which carry a high mortality rate. Older patients or those with medical comorbidities are at greater risk for severe disease. Inflammation, pulmonary edema and an over-reactive immune response can lead to hypoxia, respiratory distress and lung damage. Mesenchymal stromal/stem cells (MSCs) possess potent and broad-ranging immunomodulatory activities. Multiple in vivo studies in animal models and ex vivo human lung models have demonstrated the MSC’s impressive capacity to inhibit lung damage, reduce inflammation, dampen immune responses and aid with alveolar fluid clearance.
Additionally, MSCs produce molecules that are antimicrobial and reduce pain. Upon administration by the intravenous route, the cells travel directly to the lungs where the major- ity are sequestered, a great benefit for the treatment of pulmonary disease. The in vivo safety of local and intravenous administration of MSCs has been demonstrated in multiple human clinical trials, including studies of acute respiratory distress syndrome (ARDS). Recently, the application of MSCs in the context of ongoing COVID-19 disease and other viral respiratory illnesses has demonstrated reduced patient mortality and, in some cases, improved long-term pulmonary function. Adipose-derived stem cells (ASC), an abundant type of MSC, are proposed as a therapeutic option for the treatment of COVID-19 in order to reduce morbidity and mortality. Additionally, when proven to be safe and effective, ASC treatments may reduce the demand on critical hospital resources. The ongoing COVID-19 outbreak has resulted in significant healthcare and socioeconomic burdens across the globe. There is a desperate need for safe and effective treatments. Cellular based therapies hold great promise for the treatment of COVID-19. This literature summary reviews the scientific rationale and need for clinical studies of adipose-derived stem cells and other types of mesenchymal stem cells in the treatment of patients who suffer with COVID-19.
Keywords: COVID-19, SARS-CoV-2, ARDS, Pneumonia, Mesenchymal stem cells
Regenerative Medicine: Survival Strategies
Laxmaiah Manchikanti, MD
American Society of Interventional Pain Physicians (ASIPP), Paducah, KY
In the modern COVID era, regenerative medicine is facing multiple issues. In this discussion, we will present:
-
Stem Cell Therapy
-
Chaos and Uncertainty
-
21st Century Cures Act
-
FDA Role
-
Survival Strategies
The chaos continues to multiply in the United States with multiple opinions, closing of clinics, and overall abuse of therapy. Consequently, uncertainty continues to play a major role. This has led the FDA to issue multiple statements, questions, and closure of various clinics and the development of INDs. The FDA clarified the role of stem cell therapy as follows:
-
The safety and efficacy of the use of stem cells derived from peripheral blood or bone marrow for hematopoietic reconstitution are well established.
-
Stem cells derived from sources such as adipose tissue are being used to treat multiple orthopedic, neurologic, and other diseases.
- Often, these cells (whether derived from autologous or allogeneic sources) are being used in practice based on minimal clinical evidence of safety or efficacy.
The FDA has issued multiple newer regulations. At the present time, we are even concerned that clinical use of bone marrow may require in the future an IND and may not be defined as the same surgical procedure and meeting minimal manipulation and homologous use.
Consequently, we have developed a position statement for bone marrow use in musculoskeletal and spine conditions.
To preserve stem cell therapy, or specifically bone marrow concentrate therapy in musculoskeletal and spine conditions, we have to approach carefully with education, advocacy, certification, guidelines, and outcomes registry.
In multiple manuscripts published starting with safe, responsible, and effective use of stem cells in low back (Navani A, Manchikanti L, Albers SL, et al. Responsible, safe, and effective use of biologics in the management of low back pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician 2019; 22:S1-S74), BMC position statement (Manchikanti L, Centeno CJ, Atluri S, et al. Bone marrow concentrate (BMC) therapy in musculoskeletal disorders: Evidence-based policy position statement of American Society of Interventional Pain Physicians (ASIPP). Pain Physician 2020; 23:E85-E131) , and a systematic review by Sanapati et al (Sanapati J, Manchikanti L, Atluri S, et al. Do regenerative medicine therapies provide long-term relief in chronic low back pain: A systematic review and metaanalysis. Pain Physician 2018; 21:515-540), we have clarified the very important need for producing appropriate literature and disseminating them.
Spine Nerve Root Injections with PRP: Novel Approach
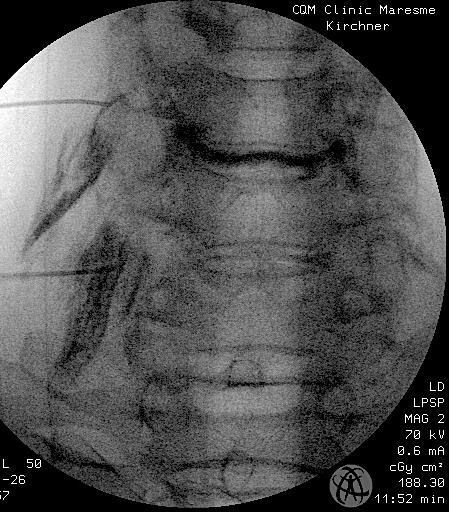
Fernando Kirchner, MD
Orthopaedic Surgeon, Institute of Traumatology Barcelona (ITB), SPAIN
The evolution in the knowledge of the degenerative processes in the spine that occur over the years and their pathophysiology leave as a result: 1) Intervertebral Disc (IVD) degeneration and its lesions (Annular fissures, disc hernia/protrusion or disc extrusion); 2) alteration of the Functional Vertebral Unit (FVU) and its lesions (Zygapophyseal osteoarthritis and disc degeneration); 3) Schmorl hernias in the vertebral endplate (VEP) and 4) VEP chronic fractures and fissures that alter the disc nutrition.1-3
The knowledge of all these processes has led to a deep research on the response of different therapeutic agents to slow down the natural evolution of disc degeneration.3 Prominent among these is PRGF infiltration,^3, 4^ that our group has been performing for 10 years through minimally invasive techniques, both in lumbar and cervical spine.
Starting from an action protocol with strict inclusion and exclusion criteria, more than 1300 protocols have been carried out which have been evaluated through pre and 6/12/24-months post MRI (Fig.1), Numerical Rating Scale (NRS) and quality of life and pain questionnaires such as Spine COMI and OSWESTRY. We highlight the improvement of neuritic pain (Fig.2) and pain caused by mechanical overload in the FVU, and the permanent improvement in the degenerative process of the disc and endplate.5
Keywords: platelet-rich plasma, regenerative medicine, orthopedics, osteoarthritis, interventional spine
References
-
Fardon D. Nomenclature and Classification of Lumbar Disc Pathology. Spine. 2001; 26(5):461-462.
-
Huang Y, Urban J, Luk K. Intervertebral disc regeneration: do nutrients lead the way? Nat Rev Rheumatol. 2014; 10(9):561-566.
-
Anitua E, Padilla S. Biologic therapies to enhance intervertebral disc repair. Regen. Med. 2018; 13(1):55-72.
-
Wang S, Rui Y, Tan Q, Wang C. Enhancing intervertebral disc repair and regeneration through biology: platelet-rich plasma as an alternative strategy. Arthritis Res Ther. 2013; 15(5):220.
-
Kirchner F, Anitua E. Intradiscal and intra articular facet infiltrations with plasma rich in growth factors reduce pain in patients with chronic low back pain. J Craniovertebr Junction Spine. 2016; 7(4):251.
Higher Concentration Intradiscal PRP: a retrospective clinical outcome study
Gregory E. Lutz, MD Regenerative SportsCare Institute New York, NY
Intradiscal Platelet Rich Plasma (PRP) is a promising orthobiologic treatment for patients with chronic lumbar discogenic pain. Preliminary reports of lower concentration (3-5X) PRPs have shown moderate pain relief and functional improvement. The purpose of our study was to investigate whether a higher dose (12-15X) PRP would improve clinical outcomes. We retrospectively reviewed our intradiscal orthobiologic registry of 192 patients to select out 45 patients who underwent isolated higher dose intradiscal PRP and met our inclusion/exclusion criteria. An independent observer collected pain, function, and patient satisfaction data, on 37/45 patients (82% follow-up rate) with an average age of 42.7 years (range 14-75) and an average follow-up time of 18.3 months (range 2-44 months). We then compared our data to historic data of a similar group of patients treated with the lower dose PRP. The results revealed a greater degree of pain relief (3.4 vs 1.7 VNS mean change), a greater degree of functional improvement (46.4 vs 33.7 FRI mean change) and a greater percentage of satisfied patients (81% vs 55%) when compared to the historic control data. Respecting the limitations inherent in a retrospective study of this nature, there appears to be a clinical benefit to using a higher concentration intradiscal PRP in patients with chronic lumbar discogenic pain.
OrthoBiologics for Grade II Tendinopathies from Animals to Humans: Evidence Based Medicine
Sherman O. Canapp Jr., DVM, MS, CCRT Diplomate, American College of Veterinary Surgeons
Diplomate, American College of Veterinary Sports Medicine & Rehabilitation (Past President)
From animals to humans, Grade 2 tendinopathies are extremely common. While there are numerous treatment options for these types of tendinopathies, they are often frustrating as recurrence is not uncommon.
In both animals and humans, classic literature has reported physical therapy, nonsteroidal anti-inflammatory drugs, and corticosteroid injections as the mainstay of treatment but are not optimal given that most tendon disorders seem to involve degenerative changes in addition to inflammation. Due to the relatively acellular and avascular nature of tendon as well as the change of tendon microenvironment after injury, tendon repair is slow and often incomplete (dysfunctional repair response).
The inability of tendon to self-repair and the inefficiency of current treatment regimens used clinically have sparked the exploration of alternative treatment strategies. Both in animals and humans the field of orthobiologics has taken the forefront, and various treatments have been developed and explored including the use of platelet rich plasma (PRP), Bone Marrow Aspirate Concentrate (BMAC), mesenchymal stem cells (MSCs), and amnionic fluid.
In this presentation, the translational approach (animals to humans and humans to animals) for the use of orthobiologics for the treatment of Grade 2 tendinopathies will be explored.
Ulnar Collateral Ligament Treatment with Platelet Rich Plasma and Bone Marrow Concentrate in the Throwing Athlete
Luga Podesta, MD
The Bluetail Medical Group-Naples, 1201 Piper Boulevard, Naples, FL 34110
Introduction: Studies have demonstrated that a leukocyte rich-platelet rich plasma (LR-PRP) is an effective option to successfully treat grade 1 and 2 partial tears of the ulnar collateral ligament (UCL) in the throwing athlete. To date, there are no published reports of long-term clinical outcomes of partial ulnar collateral ligament (UCL) tears of the elbow treated with LR-PRP or the effectiveness of treating more chronic and severe grade 2 tears or partial distal UCL tears with a combination of a single injection LR-PRP and bone marrow concentrate derived progenitor cells. The purpose of this study is to first, evaluate the long-term clinical outcome of patients who have undergone a single LR-PRP injection for treatment of a partial ulnar collateral ligament tear and second, report preliminary results of our ongoing study treating UCL injuries with a single injection of a combination LR-PRP and BMC derived progenitor cells in high demand pitchers with more severe injuries.
Methods: Twentynine of our original 30 patients treated with a single LR-PRP for a partial tear of the UCL that had returned to throwing at the same level of competition or higher from 2010 to 2020 were reviewed. Each completed an outcome questionnaire asking: How long did you continue to throw at the same level of competition or better after treatment, Did you experience any recurrence of medial elbow pain, did you sustain a recurrence or new UCL injury after returning to throw, did you retire from baseball as a result of a new or recurrent injury to the UCL?
The initial twenty-eight high demand, elite high school and collegiate pitchers, average age 18.5 years with acute and or chronic, higher grade-2 partial thickness or distal ulnar collateral ligament tears confirmed on MRI were prospectively followed from 2015 through 2020. All patients had failed at least two months of conservative treatment and an attempt to return to play. Baseline questionnaires, including the Kerlan Jobe Shoulder and Elbow Score (KJOC Score) and Disability of the Arm, Shoulder, and Hand Score (DASH Score) were completed for each patient prior to injection. Baseline ultrasound measurement of the humeral-ulnar joint space was also assessed with 10 pounds of valgus stress on the elbow. Each patient underwent a single LR-PRP combined with BMC injection of the entire ulnar collateral ligament under ultrasound guidance. All patients with distal tears and high grade-2 tears were braced for 3 weeks post treatment. All injections were performed by the same treating physician at a single institution. The same system for PRP and BMC preparation was used with each of the injections. Patients completed a course of supervised physical therapy and were allowed to return to play based on their symptoms, physical examination and dynamic ultrasound evaluation. Outcome scores, including KJOC and DASH Scores, were collected after return to play and were compared with baseline scores. Ultrasound measurements were collected at 6 weeks, 10 weeks, 14 weeks and final follow-up and compared with pre-injection values.
Results:
LR-PRP: After a single LR-PRP, 29 of the original 30 athletes that returned to competitive throwing, continued to throw for 4 years at the same level of competition or better without recurrence of injury or new UCL tear. Ten athletes continued to play for 8 years at the same level or higher of competition. 28 athletes went on to play recreationally after their competitive careers ended. One athlete sustained a shoulder injury after returning to play, forcing his retirement from competitive play. None of the original 30 participants in this study experienced a recurrence of their UCL injury, a new
UCL injury or where forced to retire from competitive baseball as the result of their original UCL injury.
LR-PRP + BMC: Preliminary results to date showed, 28/28 patients returned to throwing 7 weeks post treatment, and returning to pitching at the same level of competition or higher, between 12-14 weeks. All 28 pitchers are currently pitching over 3 years at the same level of competition or higher without pain, recurrence or new UCL injury.
One patient ruptured his UCL 2 years 4 months after his initial treatment with LR-PRP and BMC. Prior to his new injury, he had grown 6 inches in height and increased his fastball velocity over 10 mph.
Key Observations: After 10 years of treating high-level throwers biologically with these injuries, I have made several key observations important for optimal outcome: 1. Using the appropriate biologic graft for a specific injury is extremely important, 2. Knowledge of the chronicity, severity and location of the injury is necessary to select the appropriate orthobiologic graft, 3. Guidance is necessary to deliver the orthobiologic directly into the damaged ligament, 4. Post treatment rehabilitation progression early on allowing for graft absorption and natural healing cascade, leading eventually to returning to throw are of equal importance, 5. The use of dynamic ultrasound evaluation, quantitating ligament healing and joint stabilization at key times during recovery is absolutely necessary to safely introduce valgus exercise progressions and eventual return to throwing.
Conclusion: The results of this ten-year follow-up of our original PRP study, confirms that a single injection of LR-PRP may beis an effective option to successfully treat partial ulnar collateral ligament tears of the elbow in athletes.
Preliminary results of performing a single injection combining LR-PRP + BMC is also an effective option to successfully treat more significant partial ulnar collateral ligament tears of the elbow in higher demand athletes with more significant and or distal UCL injuries.
References
-
Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689-1694.
-
Mishra A, Harmon K, Woodall J, Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol. 2012;13(7): 1185-1195.
-
Deal JB, Smith E, Heard W, O’Brien MJ, Savoie FH 3rd. Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthop J Sports Med. 2017;5(11): 2325967117738238.
-
Dines JS, Williams PN, ElAttrache N, et al. Platelet-rich plasma can be used to successfully treat elbow ulnar collateral ligament insufficiency in high-level throwers. Am J Orthop 2016;45(5):296-300.
-
Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15-17.
-
Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723-728.
-
O’Holleran JD, Altcheck DW. The throwers elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J 2006; 2:83-93.
-
Werner SL, Fleisig GS, Dillman CJ Andrews JR. Biomechanics of the elbow during baseball pitching. J Orthop Sports Rhys. Ther 1993; 17:274-278.
-
Nazarian LN, McShane JM, Ciccotti MG, O’Kane PL et al, Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major-league baseball pictures. Radiology 2003; 227:148-154.
-
Sasaki J, Takahara M, Ogino T, et al. Ultrasonographic assessment of the ulnar collateral ligament and medial elbow laxity in college baseball players. J Bone Joint Surg. Am. 2002; 84:525-531. 2002
-
Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67-83.
-
Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158-1163.
Ethical and Compliant Practice and Marketing of Orthobiologics
Joanne Halbrecht, MD
CDA Orthopedics and Sports Medicine, Coeur d’Alene, ID
The use of biologics for orthopedic pathology is rapidly increasing. Food and Drug Administration (FDA) Guidance and the Federal Trade Commission (FTC) govern how industry and practitioners use and market these products. Practitioners are also subject to ethical parameters defined by their respective certifying and licensing bodies. A recently published study identified 896 stem cell clinic websites, 96% of which gave consumers misinformation. Ethical and compliant use and marketing of orthobiologics instills patient trust, ensures product safety, avoids medical complications and protects the practitioner from medical society and licensing reprimand and litigation.
Peptide Signaling for Cellular Efficiency and Reduction of Senescence: Optimizing Autologous BMC and PRP
William Seeds, MD
Spire Institute, Olympic Training Center, Geneva, OH
Improved cellular efficiency has the ability to promote favorable outcomes for degenerative joint disease regardless of the etiology. Metabolic flexibility of the cell modulates interaction of cell metabolism and 2 way communication with the innate and adaptive immune system. Loss of metabolic flexibility leads to changes in thermodynamic ratios of nucleotide coenzyme couples NAD/NADH, NADP/NADPH, ADP/ATP and AcetylCoA/CoA in the mitochondria and cell cytoplasm disrupting cellular homeostasis. Theses cellular changes in redox and altered mitochondrial function decreases the cells ability to maintain adequate antioxidant transcription.
Increasing Oxidative stress overtakes the cellular capacity for DNA damage for repair, autophagy and mitophagy . P53 tumor suppressor is a master regulator in maintaining cellular Redox, efficiency and immune cell interaction. P53 controls cellular progression to the proinflammatory state of irreversible Senescence Associated Secretory Phenotype (SASP) or to cellular apoptosis. Stem cells are vital for repair and require quiescence for activation. Stem cell senescence alters cell repair potential and favors continued disease progression. Peptide therapies offer natural, non-toxic directed cell signaling to alter redox, initiate stem cell migration offer senomodulating and senolytic potentials. The peptide AOD9064 was used in combination with HA and significantly improve symptoms of osteoarthrosis if the knee.
References
Fafián-Labora JA, Morente-López M, Arufe MC. Effect of aging on behavior of mesenchymal stem cells. World J Stem Cells. 2019;11(6):337-346.
Amniotic Suspension Allograft Improves Pain and Function in Both In Vivo and Clinical Studies
Jack Farr, MD[3], Andreas H. Gomoll[4], Kelly A. Kimmerling[5], Katie C. Mowry[6]
Introduction: Amniotic suspension allograft (ASA) is composed of cells from the amniotic fluid and micronized amniotic membrane, consisting of regenerative and anti-inflammatory cytokines and growth factors. A pilot study utilizing ASA as an intra-articular treatment for osteoarthritis (OA) demonstrated safety and showed trends for improved pain and function scores. In order to further elucidate results, two OA animal models were utilized (monosodium iodoacetate: MIA; medial meniscal tear: MMT). In these models, we measured pain and function using behavioral testing, histological assessment of joints, and synovial fluid biomarkers. Additionally, a multicenter randomized, controlled clinical trial was completed comparing ASA to hyaluronic acid (HA) and saline to evaluate the efficacy of ASA for OA symptom modification out to 12 months.
Methods: Animal studies: MIA was injected into the right knees of rats (day 0); on day 7, 50μL of ASA, saline, or triamcinolone was injected. Rats were sacrificed on day 21, and synovial fluid was collected for biomarker analysis. For the MMT study, the medial meniscus was transected (day 0); on day 7, 50μL of ASA, vehicle control, or FGF18 was injected. Rats were sacrificed on day 17 or day 28; synovial fluid was collected for biomarker analysis. For both MIA and MMT studies, behavioral testing including pain threshold (Von Frey), incapacitance, swelling, and gait analysis was conducted. Histological assessment of joint quality (both) and microCT imaging for cartilage degradation (MMT only) were also completed.
Clinical study: 200 patients were randomized (across 12 sites) 1:1:1 to one of three treatment arms: saline, HA, or ASA. Patient reported outcomes (PROs) were completed at baseline, 1 week, 6 weeks, 3 months, 6 months, and 12 months following injection. Changes in Visual Analog Scale (VAS) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) from baseline were used to assess efficacy of the injection. Mixed models of repeated measures (MMRM) was used to calculate statistics.
Results: In the MIA and MMT study, rats had significantly higher pain thresholds compared to the vehicle control (p<0.05) and reduced weight bearing differences (incapacitance, p<0.05) following treatment with ASA. In the MIA study, treatment with ASA significantly reduced swelling (p<0.01), while in the MMT study, ASA treatment significantly improved gait scores (p<0.05). Additionally, synovial fluid biomarker analysis revealed significantly increased levels of IL-10 (p<0.05) in both studies with ASA treatment. These results correlate with what was seen clinically; at 12 months post-injection, patients receiving ASA showed significantly lower VAS joint pain scores compared to both HA and saline (p<0.001, p<0.01, respectively). For the KOOS pain subscale, patients receiving ASA had significantly better scores compared to both HA and saline at 12 months (p<0.01). For KOOS activities of daily living, ASA treatment resulted in significant increases compared to both HA and saline (p<0.01, p<0.05, respectively) at 12 months.
Conclusions: In this 200-patient multicenter randomized, controlled trial, patients receiving ASA showed greater improvements in pain and function compared to HA and saline; these results were supported from the two pre-clinical rat studies using the MIA and MMT OA models. These studies all provide evidence for the use of ASA for OA symptom modification.
Effect of the stellate ganglion block treatment on posttraumatic stress disorder: a randomized clinical trial
Sean Mulvaney, MD
Regenerative Orthopedics & Sports Medicine, Annapolis MD
This brief lecture is a discussion of this level 1 multi-center randomize clinical trial recently published in a high-impact medical journal. PTSD is a highly prevalent condition significantly that impacts many patients seen in a musculoskeletal clinical setting. Many of the standard treatments have only modest efficacy per the medical literature. SGB is safe, highly tolerated, and effective. In addition to this level 1 study, over the last 10 years there are at least 18 publications in the medical literature showing safety and efficacy.
Exosomes 101: Ready for Prime Time? Marrow Derived Plasma: Undervalued Role in Regulating Inflammation
Ryan Dregalla
Napa Medical Research Foundation, Napa, CA
Exosomes are unique nanoparticles/vesicles generated by numerous cell-types, play an ancillary role in intercellular communication and are found in various biological fluids.^1, 2^ Exosomes fuse with the membrane of a target cell and alters its function by delivering RNAs (e.g. m-, si-, mi-, mt-), DNA and peptides/proteins.2 These nanoparticles are highly heterogenous with respect to size, surface markers and intra-vesicular constituents.2 The distinct role(s) and physiological regulation of exosomes is not elucidated and are known to both: protect against and accelerate/promote disease.3
Recently, allogenic exosomes have entered the field of orthobiologics as a potential method for reducing inflammation and promoting anabolic processes based on the findings of in vitro and animal models. While several of these studies have shown exciting results, they required supra-physiological levels of ex vivo-generated exomes and human data is lacking.3-5 Exosomes hold tremendous promise as a future orthopedic therapy, but they are not generically beneficial or homologous. Significant research is required to determine the clinical considerations for exosome therapy (e.g. cell-targeting, dosing) and how to engineer/source these nanoparticles to possess the constituents necessary to achieve the desired outcome with safety and efficacy.
References
-
van Niel, G., D’Angelo, G. & Raposo, G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol 19, 213-228, doi:10.1038/nrm.2017.125 (2018).
-
Kalluri, R. & LeBleu, V. S. The biology, function, and biomedical applications of exosomes. Science 367, doi:10.1126/science.aau6977 (2020).
-
Li, J. J., Hosseini-Beheshti, E., Grau, G. E., Zreiqat, H. & Little, C. B. Stem Cell-Derived Extracellular Vesicles for Treating Joint Injury and Osteoarthritis. Nanomaterials (Basel) 9, doi:10.3390/nano9020261 (2019).
-
Mao, G. et al. Exosomes derived from miR-92a-3p-overexpressing human mesenchymal stem cells enhance chondrogenesis and suppress cartilage degradation via targeting WNT5A. Stem Cell Res Ther 9, 247, doi:10.1186/s13287-018-1004-0 (2018).
-
Thery, C. et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles 7, 1535750, doi:10.1080/20013078.2018.1535750 (2018).
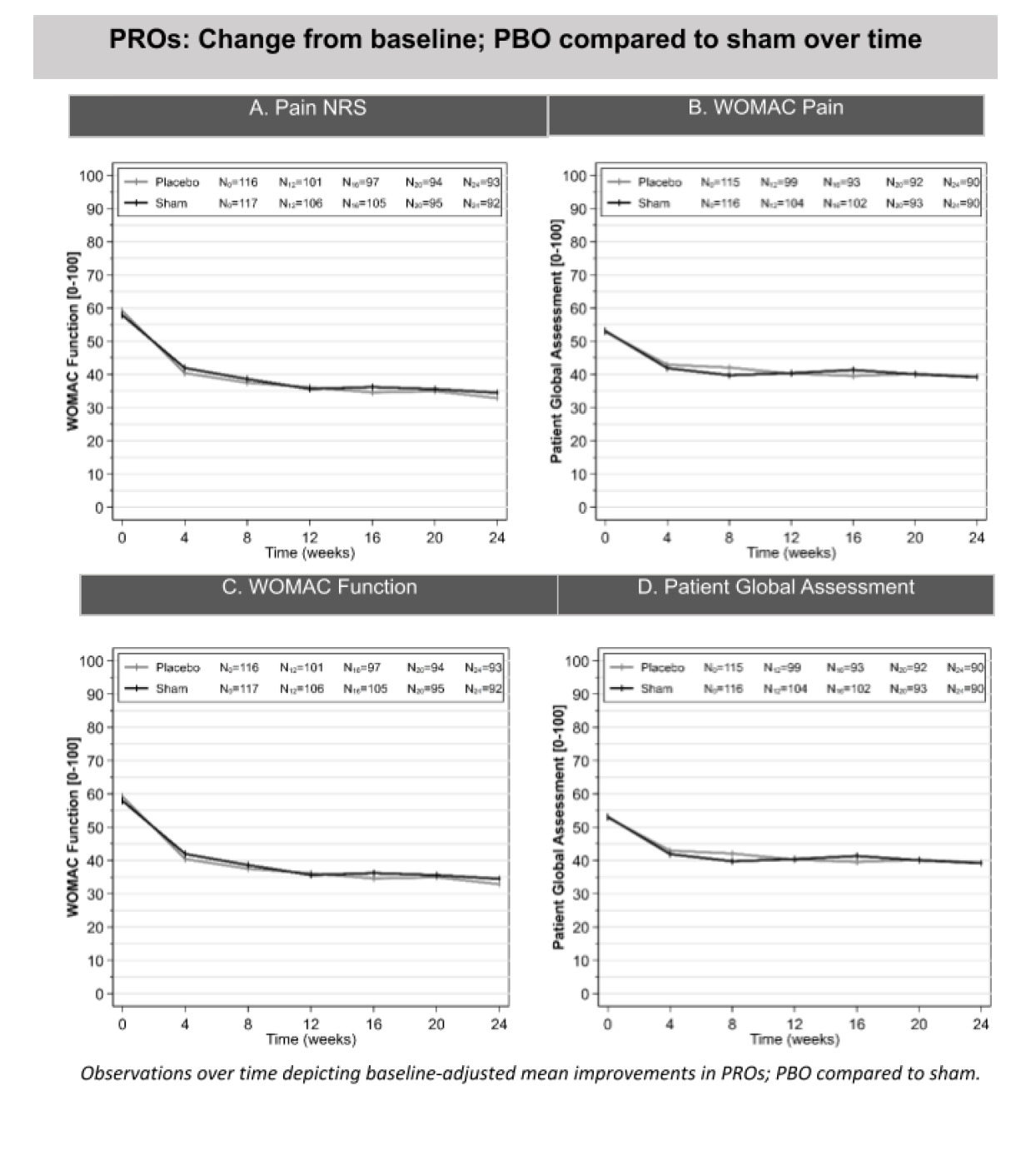
The Placebo Effect: Intraarticular Normal Saline Vs Dry Needle Sham Injection in Knee Osteoarthritisx
Anne Marie Tilton
Senior Medical Science Liaison, Samumed, Chicago, IL
Yusuf Yazici, MD[7], Jeyanesh Tambiah, MD[8], Christopher Swearingen, PhD[9], Annemarie Tilton, MD[10], Sarah Kennedy, PhD[11], Vibeke Strand, MD[12], Brian Cole, MD, MBA[13]
Objective: To compare the effects of saline and sham (dry needle) intra-articular injections on symptoms in subjects with knee osteoarthritis (OA).
Design: Double-blind, randomized controlled trial
Setting: Multicenter trial in the United States
Participants: Adults with symptomatic, mild to moderate knee OA
Interventions: Single intra-articular knee injection of saline or sham (dry needle)
Main outcome measures: Change from baseline to Week 24 in the weekly averages of the following patient-reported outcomes (PROs): Pain Numeric Rating Scale (Pain NRS; 10-point visual analog scale), WOMAC Pain, WOMAC Function, and Patient Global Assessment (PtGA).
Level of evidence: Level 2, randomized controlled trial
Results: 207 out of 233 subjects in the saline and sham arms completed the 24-week study. Both the saline and sham groups reported clinically relevant improvements (>10%) in all PROs relative to baseline (Figure). These improvements were evident at Week 1 and lasted through Week 24. Between the saline and sham groups, no clinically or statistically significant differences in PROs were seen at any time points during the study.
Conclusion: Knee OA subjects who received a saline injection reported similar changes in their symptoms over 24 weeks as those who received a sham injection (measured by Pain NRS, WOMAC Pain, WOMAC Function, and PtGA). While it has been suggested that placebo effects in knee OA trials could be due to therapeutic effects of saline in the joint, these results demonstrated that patients experienced similar effects with the insertion of a dry needle into the knee. As a result, these putative saline placebo effects appeared related to the contextual effects of having a knee injection procedure rather than from direct effects of saline in the joint.
Integrating Extracorporeal Shock Wave Therapy (ESWT) with PRP Patient Outcomes Data
Nicola Maffulli, MD
Queen Mary University of London, London, United Kingdom
In the United Kingdom, soft tissues disorders have a prevalence of 18 cases for 1,000 individuals, and account for 40% of new rheumatology consultations. Tendons can undergo degenerative and traumatic processes, indeed, most vulnerable tendons are those of the rotator cuff, the long head of the biceps, the wrist extensors and flexors, the adductors, the posterior tibial tendon, the patellar tendon and the Achilles tendon, commonly secondary to overload, and one third of patients with these pathologies do not practice intensive physical activity.
Tendon injuries can be acute or chronic and caused by intrinsic (age, body structure, nutrition, metabolic diseases, genetics) or extrinsic (excessive, fatigue and improper loading disuse and external damage) factors, alone or in combination. In acute trauma, extrinsic factors predominate, whilst in chronic cases intrinsic factors also play a role.
These factors are associated with the onset of overload pathology of tendons, though there is not a specific cause - effect relationship.
Despite morbidity associated in athletes, management is far from scientifically based, and many of therapeutic options reported are lacking a hard-scientific background.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used. Although NSAIDs may provide some pain relief, they do not actually result in sustained improvement in the healing process. Among conservative management for Achilles tendinopathy more options are the extracorporeal shock-wave therapy (ESWT) and platelet-rich plasma (PRP) injections. ESWT and PRP effectiveness was reported in several studies. Both are regenerative treatments, but their mechanism of action in vivo is still unclear. The rationale to use ESWT in vivo on tendons is suggested by results obtained with shockwaves on models in vitro, such as enhancing cell proliferation, migration and secretory activity of human primary cultured tenocytes. However, in scientific literature, no evidences are reported about the best conservative management to choose for treatment of tendinopathies.
Optimizing Functional Recovery to Support Biologic Interventions in the Knee
Della Villa Francesco MD Isokinetic Medical Group, Bologna, Italy
In the last decade, a growing body of evidence has emerged regarding biologic interventions for patients suffering knee injuries and chronic conditions. Clinical outcomes are promising for different entities even if there is not complete agreement1 and it is still challenging to draw definitive conclusion on the effectiveness of these interventions.
One aspect that has been overlooked, clinically and scientifically, is the role of post-intervention rehabilitation to support the biologic intervention and possibly increase patient’s satisfaction on their functional outcomes. Compliance in a step-wised and goal-based rehabilitation program has been linked to better results following biologic knee cartilage procedures2 and higher return to sport following other orthopedic procedures.3 It is intuitive to think that the optimization of musculoskeletal function stands next to biologics intervention to support patients in the process of returning to activity.
In this context, narrow views should be abandoned to offer the patient the best possible treatment. The knee is a complex organ, belonging a kinetic chain as a part of the musculoskeletal system. Static and dynamic structures are equally important in guaranteeing a good and long-term joint homeostasis. As such, initial symptoms resolution is just the beginning and should be supported by adequate post-procedure intervention. If this is not carried out, the benefit for the patient risks to be limited and if the joint is re-inserted in the same biomechanical context there is theoretically the risk of a relapse of symptoms.
Orthobiologics intervention and high-quality rehabilitation should stand together to support biologically and functionally the knee injured patients. In detail, the same concept that have been widely studied in other knee domains, should be applied following an organized path of functional recovery to guarantee our patients the best chance to get back to their activity
References
-
Alex Scott, Robert F LaPrade, Kimberly G Harmon, Giuseppe Filardo, Elizaveta Kon, Stefano Della Villa et al. Platelet-Rich Plasma for Patellar Tendinopathy: A Randomized Controlled Trial of Leukocyte-Rich PRP or Leukocyte-Poor PRP Versus Saline. Am J Sports Med. 2019 Jun;47(7):1654-1661.
-
Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, Marcacci M.Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes? Am J Sports Med. 2010 Jan;38(1):68-77.
-
Della Villa F, Andriolo L, Ricci M, Filardo G, Gamberini J, Caminati D, Della Villa S et al. Compliance in post-operative rehabilitation is a key factor for return to sport after revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020 Feb;28(2):463-469.
Bone Marrow Aspirate: “Dry Tap” Clinical Implications and How to Manage
Michael Khadavi, MD
APEX Orthopedics & Sports Medicine, Overland Park, KS
Abstract: “Dry tap” bone marrow aspirations are rare but clinically significant complications in orthobiologics. This topic is discussed in the hematology/oncology literature, with implications of hypercellularity and cancer, however with no research in anorthobiologic demographic, the implication of a dry tap largely remains unknown. In this presentation, the literature and clinical implications of a dry-tap will be reviewed alongside a clinical case-report.
Suggestions for an evidence-based approach to a work-up and management for the case of dry tap will be discussed.
References
-
Humpries JE. Dry tap bone marrow aspiration: Clinical significance. Am J Hematol 1990, 35:247-250
-
Khanum F. “Dry Tap” of Bone Marrow and its Clinical Importance. P J M H S. 2009 Dec.
-
ENgeset A. Incidence of ‘dry tap’ on bone marrow aspirations in lymphomas and carcinomas. Diagnostic value of the small material in the needle. Scand J Haematol. 1979 May;22(5):417-22.
-
Ahmad SQ. Dry Tap: A diagnostic alert for underlying bone marrow pathology. J Ayub Med Coll Abbottabad. 2015 Jan-Mar;27(1):120-3.
Keywords: knee osteoarthritis, orthobiologics, bone marrow aspirate concentrate BMAC
Serum Sickness from PRP Injection
Brain Shiple, DO
The Center for Sports Medicine, Springfield, PA
65 yowm work out enthusiast received several PRP treatments to his arthritic ankle and failed bicep tendon insertion grafts. Each time he received a double spin suspension method of PRP with ACDA concentrated to over 1 million platelets per microL. He developed an increased temperature to approximately 100 degrees Fahrenheit and flu like symptoms of body aches, fatigue etc that would last 5 to 7days and then resolve uneventfully. A laboratory workout after his initial serum sickness event revealed no abnormalities. He still experienced decreased pain and increased function after his PRP treatments as expected. This did not occur with bone marrow concentrate or amniotic membrane graft treatmentss. We stopped any PRP treatments and only used amniotic membrane grafts going forward for any soft tissue or arthritic regen med treatments with good results and no abnormal immune reaction. I don’t know why he developed serum sickness to his own PRP. Possibly the ACDA?
Bone Marrow Concentrate (BMC) 5 Year Outcomes Data
M&M: P. Acnes Septic Joint Following BMC/PRP for Shoulder Osteoarthritis
Kristin Oliver, MD
Regenerative Orthopedics Specialist & Sports Medicine Blue Tail Medical Group, Chesterfield, MO
Knee osteoarthritis is a leading cause of pain and disability worldwide. Non-surgical treatment options are limited. The potential for cellular based regenerative therapies to bridge the gap between short-term symptomatic relief and total knee arthroplasty has received abundant attention. This presentation includes pain and functional outcomes data on 1450 patients with knee osteoarthritis treated with intra-articular bone marrow concentrate. 52 of these patients are out 5 years from the date of treatment.
Treatment registry data for 1450 patients diagnosed with Kellgren-Lawrence Stage 2-4 knee osteoarthritis were analyzed. Data regarding adverse events, Visual Analog Pain Scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index metrics (WOMAC) were obtained at intervals up to 5 years.
Adverse events were limited to transient pain and swelling of the treated joint. The mean reported WOMAC changes from pre-procedure to two years post-procedure were as follows: Pain + 24, Stiffness +25 and Function + 20. The mean reported VAS was reduced from 4.7 at baseline to 2.3 at five years.
This study of intra-articular autologous bone marrow concentrate in patients diagnosed with knee osteoarthritis demonstrates encouraging results for positive outcomes without complication.
Spondylodiscitis After Intradiscal Platelet Rich Plasma: a case report
Gregory E. Lutz, MD
Regenerative SportsCare Institute New York, NY
A 40 year old female with 2 years of chronic refractory lumbar discogenic pain underwent a leukocyte-poor intradiscal PRP injection at L5-S1. Post-procedure she developed crescendo pain with associated fever and night sweats. An MRI was performed suggestive of spondylodiscitis and a CT-guided biopsy was performed. Samples cultured grew out Cutibacterium Acnes. The patient was treated with 6 weeks of intravenous antibiotic therapy. Spondylodiscitis is a potential complication of intradiscal PRP. Future studies of the type of PRP and other strategies to mitigate against this complication will be discussed.
Minimum 12-month Clinical Outcomes of a Combined Intraosseous and Intraarticular Treatment of Knee Osteoarthritis with Autologous BMC
Mitchel Sheinkop Cellular Orthopedics, Chicago, IL
Building on the foundational work of Dr. Hernigou, the current study was structured to assess the safety and potential therapeutic benefit of treating patients with mild to moderate knee osteoarthritis with a split injection of BMC, such that approximately 80% of the injectate was delivered intraosseous to the tibial plateau, and 20% was delivered intraarticular. Each BMC preparation was analyzed for Total Nucleated Cells (TNC), and culture-based Colony Forming Units-Fibroblast (CFU-F; as a biomarker of mesenchymal signaling cells, MSCs), CFU-Osteogenic (CFU-O; as a biomarker of osteogenic progenitor cells) and CFU-Chondrogenic (CFU-C; as a biomarker of chondrogenic progenitor cells). Clinical outcomes were recorded for Knee Society Score-Function (KSS-Function), Knee Society Score-Knee (KSS-Knee), Lower Extremity Functional Scale (LEFS) and Visual Analog Scale (VAS), and assessed for correlations with patient factors, including cellularity (TNC and CFUs) and pre-treatment clinical outcome values.
Outcomes with Intraosseous BMAC and Demineralized Bone Matrix for Bone Marrow Lesions of the Knee
Bert R. Mandelbaum MD DHL
Cedars-Sinai Kerlan-Jobe Institute, Los Angeles, CA
Osteochondritis dissecans , Osteonecrosis and other Bone Marrow lesions of the knee are avascular processes of subchondral bone that can ultimately result in fragmentation and eventual separation of the unhealthy bone and cartilage to produce a loose body, create an associated osteochondral defect.1 This has the potential to lead to early osteoarthritis and the associated morbidity that comes with it.2,3
The standard treatment for these processes of the knee is either a transarticular or retroarticular drilling procedure. The philosophy of these procedures is to create vascular channels that will allow blood and marrow elements to egress into the diseased bone and gradually replace it with healthy bone.4In an effort to accelerate healing and obtain more reliable and complete normalization of radiographs, a new procedure called Bioplasty .This procedure uses known orthopedic techniques in combination with orthobiologic augmentation with bone marrow aspirate concentrate (BMAC) and sometimes is mixed with a bone scaffold, typically demineralized bone matrix (DBX) putty to accelerate and stimulate healing.
This novel procedure represents a paradigm shift for treatment .Traditional drilling procedures, either trans or retroarticular, attempt to heal a Bone Marrow Lesion via a method of creeping substitution in which channels are created from the unhealthy bone. This allows blood and marrow elements to egress into the unhealthy bone and gradually revascularize it and replace it with healthy bone. Several studies have reported on the efficacy of traditional drilling procedures with success rates of 80-90%.5-8 However, the process of creeping substitution is slow and the average healing time has been reported to be as long as 11 months for larger lesions and the definition of healing in these prior reports remains controversial.9-13
Biologic stimulation with a scaffold (BMAC mixed with bone graft) is placed to fill in the cavity in order to stimulate bony reconstitution of the cavity. Core decompression with biologic stimulation has been performed successfully for avascular necrosis (AVN) of the femoral head as well as spontaneous osteonecrosis of the knee (SONK) with good results.11,12
This procedure follows the same logic as core decompression of the femoral head and condyles–it allows for complete removal of the lesion rather than relying on the slow and sometimes unreliable process of creeping substitution. Utilization of BMAC to biologically stimulate and accelerate healing and bone graft integration has been shown to be safe and effective in both animal models and in clinical trials.13,14
References
-
Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181-91.
-
Hefti F, Beguiristain J, Krauspe R, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8(4):231-45.
-
Edmonds EW, Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from König to the ROCK study group. Clin Orthop Relat Res. 2013;471(4):1118-26.
-
Heyworth BE, Edmonds EW, Murnaghan ML, Kocher MS. Drilling techniques for osteochondritis dissecans. Clin Sports Med. 2014;33(2):305-12.
-
Anderson AF, Richards DB, Pagnani MJ, Hovis WD. Antegrade drilling for osteochondritis dissecans of the knee. Arthroscopy. 1997;13(3):319-24.
-
Boughanem J, Riaz R, Patel RM, Sarwark JF. Functional and radiographic outcomes of juvenile osteochondritis dissecans of the knee treated with extra-articular retrograde drilling. Am J Sports Med. 2011;39(10):2212-7.
-
Edmonds EW, Albright J, Bastrom T, Chambers HG. Outcomes of extra-articular, intra- epiphyseal drilling for osteochondritis dissecans of the knee. J Pediatr Orthop. 2010;30(8):870-8.
-
Donaldson LD, Wojtys EM. Extraarticular drilling for stable osteochondritis dissecans in the skeletally immature knee. J Pediatr Orthop. 2008;28(8):831-5.
-
Wall EJ, Milewski MD, Carey JL, et al. The Reliability of Assessing Radiographic Healing of Osteochondritis Dissecans of the Knee. Am J Sports Med. 2017;45(6):1370-1375.
-
Haeri hendy S, De sa D, Ainsworth K, Ayeni OR, Simunovic N, Peterson D. Juvenile Osteochondritis Dissecans of the Knee: Does Magnetic Resonance Imaging Instability Correlate With the Need for Surgical Intervention?. Orthop J Sports Med. 2017;5(11):2325967117738516.
-
Shah SN, Kapoor CS, Jhaveri MR, Golwala PP, Patel S. Analysis of outcome of avascular necrosis of femoral head treated by core decompression and bone grafting. J Clin Orthop Trauma. 2015;6(3):160-6.
-
Duany NG, Zywiel MG, Mcgrath MS, et al. Joint-preserving surgical treatment of spontaneous osteonecrosis of the knee. Arch Orthop Trauma Surg. 2010;130(1):11-6.
-
Patterson TE, Boehm C, Nakamoto C, et al. The Efficiency of Bone Marrow Aspiration for the Harvest of Connective Tissue Progenitors from the Human Iliac Crest. J Bone Joint Surg Am. 2017;99(19):1673-1682.
-
Jäger M, Herten M, Fochtmann U, et al. Bridging the gap: bone marrow aspiration concentrate reduces autologous bone grafting in osseous defects. J Orthop Res. 2011;29(2):173-80.
Covington Orthopedic Sports Medicine Institute, Regenerative Medicine, Covington, LA 70433
Covington Orthopedic Sports Medicine Institute, Regenerative Medicine, Covington, LA 70433
Knee Preservation and Cartilage Restoration Center, OrthoIndy, Indianapolis, IN Department of Orthopaedic Surgery, Indiana University School of Medicine, Indianapolis, IN
Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY
Department of Research and Development, Organogenesis, Birmingham, AL
Department of Research and Development, Organogenesis, Birmingham, AL
Samumed, San Diego, CA
Samumed, San Diego, CA
Samumed, San Diego, CA
Samumed, San Diego, CA
Samumed, San Diego, CA
Stanford University School of Medicine, Palo Alto, CA
Midwest Orthopedics at Rush University, Chicago, IL

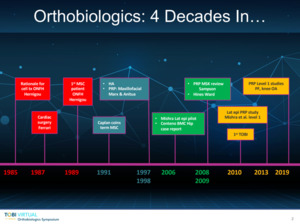



.jpeg)
.jpeg)














_pre-treatment_(2014)_(b-e)_1_year_after_tto_(c-f)_2_years_after_tto.png)
















.jpeg)
.jpeg)


















_pre-treatment_(2014)_(b-e)_1_year_after_tto_(c-f)_2_years_after_tto.png)