Introduction
Total knee arthroplasty (TKA) is the gold standard treatment for end-stage osteoarthritis with a rich body of literature and high-level evidence reporting safe, durable, and cost-effective procedure with favorable long-term outcomes (Murray et al. 2014; Courtney et al. 2016; Price et al. 2018). However, an estimated 20% of patients are dissatisfied with their outcomes. Dissatisfaction and TKA failure has been attributed to the surgeon, patient, and implant-related factors (Lombardi, Berend, and Adams 2014; Gunaratne et al. 2017). From the surgeon’s perspective, the most important variables are both surgeon-dependent and modifiable, such as technical factors (Aoki 2019; Aalen et al. 2015; Andersen et al. 2012).
Technical performance is dependent on following the guiding principles in TKA to (1) restore ligament stability, (2) successful attainment of target alignment, and (3) soft tissue-balance (Vajapey, Fitz, and Iorio 2022; Scott 2016). One modality within the surgeon’s armamentarium to ameliorate poor surgical outcomes through improved technical performance is robotic-assisted TKA (rTKA) (Riantho et al. 2023). Multiple studies have shown that robotic surgery yields improved alignment (Courtney et al. 2016; Gunaratne et al. 2017), though the systems are not error-free and the limitations of each system are unique (Siddiqi et al. 2021; Carli et al. 2014).
There is a dearth of comparative literature focused on robotic systems in TKA, and published literature is primarily individualized (Walgrave and Oussedik 2023). To our knowledge no study has explored the agreement of the intraoperative alignment obtained by the robot used to guide corrective resection and preoperative radiographic measurement. The purpose of this study is a comparative analysis of the coronal limb alignment in total knee arthroplasty between the standard preoperative radiographic measurement and intraoperative imageless robot calculations. The primary purpose of this study was to observe and quantify any differences in limb alignment measurement. Secondarily, we sought to perform an exploratory analysis of factors that bias alignment measurements, including deformity magnitude and deformity phenotype.
Methods
Patient selection
Between December 2021 and December 2022, surgeon data were prospectively collected and retrospectively reviewed for all patients who underwent knee surgery by a single fellowship-trained surgeon. Inclusion criteria included (1) primary TKA and (2) a robotically assisted TKA. Cases were excluded (1) if prospectively assessed radiographic measurements were not recorded and (2) if robotic data corruption, meaning data was not available for review secondary to an upload to the database error, occurred. Surgeon data for each patient had a unique identifier that enabled collation with robot-generated data without using unique patient identifiable data (Pijls 2023). Consequently, no patient demographic data or postoperative data are reported. This study was conducted at Valley Hospital Medical Center in Las Vegas, NV and was exempt from institutional review board oversight.
Coronal Limb Alignment
All patients had standardized preoperative radiographs (XR) that were analyzed according to the Coronal Plane Alignment of the Knee (CPAK) classification system as part of the senior surgeon’s preoperative evaluation and planning process (MacDessi et al. 2021). Radiographs included weightbearing anteroposterior and lateral knee, 45-degree semi-flexed posteroanterior knee, Merchant view, and double stance full leg anteroposterior lower limb radiographs. XR measurement of limb alignment was performed according to standard protocol, using the hip-knee-ankle (HKA) axis angle as a surrogate measure of limb alignment. HKA axis angle is performed on the double stance full leg anteroposterior lower limb radiograph with measurements in a straight line from the center of the femoral head to the center of the intercondylar notch on the femur and from the center of the tibial eminence to the center of the plafond with the angle between the two lines measured for the axis as demonstrated in Figure 1 (Bellemans et al. 2012). All radiographic measurements were assessed prospectively as part of the senior surgeon’s standard preoperative planning.
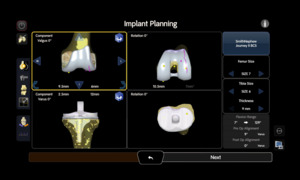
All patients underwent a standardized intra-operative alignment assessment by the senior surgeon as part of the intraoperative robotic workflow using the CORI robotic surgical system (Smith & Nephew, Inc., Memphis, TN, USA) (Murray et al. 2014). Following registration of anatomy intraoperatively, mechanical alignment and kinematic data are calculated and recorded in real-time, then electronically stored in a database according to unique surgical case identifier. Mechanical alignment assessment is derived collected from a calculated hip center, data points collected from the distal femur, proximal tibia, and medial and lateral malleoli. The mechanical axis is measured at maximum extension with application of an axial load from the heel directed cephalad to replicate weightbearing. This is done prior to removal of osteophytes and posterior cruciate ligaments. The planning screen and post-operative data screens are displayed in Figures 2a and 2b.
Statistical analysis
Descriptive statistics are reported. The primary outcome was coronal limb alignment (degrees). A secondary outcome included was deformity phenotype (varus/valgus) as an independent variable that may influence limb alignment measurement. Data points were assigned positive values for varus deformity and negative values for valgus. Varus was defined as any deviation from the neutral axis <180 and valgus >180 degrees. Bland–Altman (BA) plots and Limits of Agreement (LoA) analyses were utilized for comparative analysis of primary and secondary hypotheses and measurement agreement (Bland and Altman 1986, 1999, 2012). We differentiated statistical significance from clinical significance by data that indicated a 3 degree change in alignment had clinical consequences (Song et al. 2013). Therefore, we defined the maximum allowed difference (MAD) between measurements to 3 degrees, which implied that a LoA > MAD would indicate measurements are not in agreement. Consequently, measurements would be considered in agreement if the difference in measurements was less than a clinically significant difference (defined as 3 degrees). Alpha values of P<0.05 were considered statistically significant, and 95% confidence intervals (95CI) were reported for precision estimates. MedCalc (MedCalc Software, Ostend, Belgium) was used for statistical analysis. Figures were made with web apps (Goedhart and Rishniw 2021; Goedhart 2019).
Results
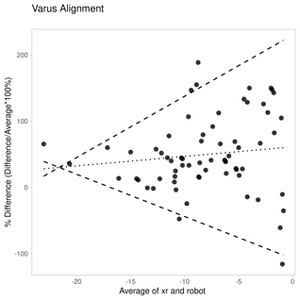
There were 258 consecutive surgical cases that met the inclusion criteria for this descriptive comparative analysis, and 212 (85%) patients had complete data available for analysis. Coronal limb alignment using XR measurement and robot calculations are reported Figure 3. The limb alignment range measured on XR was -32 to 23 degrees, and the calculated range was -17 to 17 degrees, and a -2.3-degree median difference (95CI -3.6 to -0.9) in alignment as calculated by the robot relative to radiographic measurement (Figure 3).
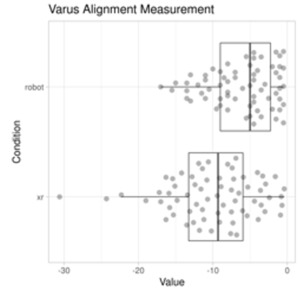
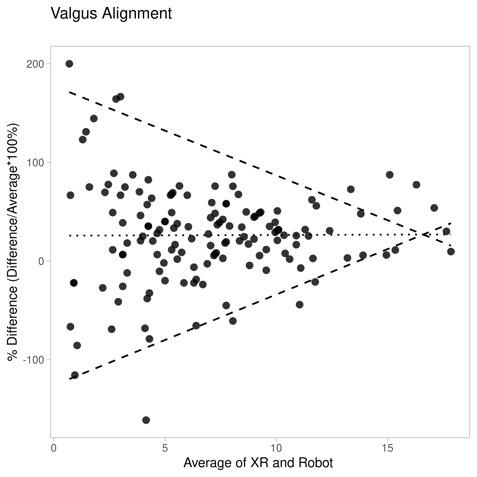
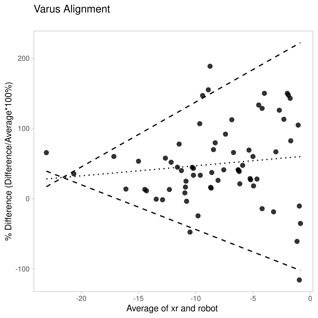
Figure 4 is a BA plot that demonstrates a systematic difference of 2.42 degrees (95CI 1.95-2.88) and with increased variability as the magnitude of alignment deformity, as demonstrated by the 0.3 (95CI 0.25-0.45) slope. Data did not meet assumptions for BA Plot due to heteroscedasticity, non-normal data, and proportional bias. Therefore, data were normalized, and regression LoA analyses were performed (Figure 4). The robot calculation systematically underestimated alignment with a -34% (95CI 26-41) difference, which increased in magnitude with increased variability as demonstrated by -0.23 (95CI -1.96-1.50) slope.
The cohort included 32% varus (67/212) and 68% (145/212) valgus knees. Robot calculation had a median -1.36 degrees (-2.9-0.2) difference compared to XR measurement for valgus knees, whereas the robot calculation had a median -4.14 (95CI 1.3-6.7) difference for varus knees. BA plot demonstrated a 26.14% (95CI 17.92 34.37) difference for the valgus cohort and 0.07 (95CI -2.07-2.20) slope, whereas the varus cohort demonstrated a 49.6% (95CI 35.5-63.7) difference and 1.44 (95CI -1.5-4.4) slope.
Discussion
Our results suggest disagreement between XR and robot measurements of limb alignment. The primary hypothesis was supported, and we found disagreement between coronal limb alignment measured on XR using the HKA axis angle as a surrogate for mechanical alignment and the intraoperative alignment calculated by the robot. The secondary hypotheses were supported, given the magnitude of deformity and phenotype of deformity differentially influence measurement bias.
There is no standardized methodology for the assessment of coronal limb alignment limb nor best alignment strategy (Vajapey, Fitz, and Iorio 2022; MacDessi et al. 2023; Matassi et al. 2023), though rTKA has consistently been reported to improve accuracy and reduce outliers with regard to reconstituting mechanical axis as measured in coronal plane (Mannan et al. 2018). Nevertheless, XR measurement of HKA axis angle has been widely adopted in clinical practice and the literature (Gieroba et al. 2023; Kort et al. 2022). In our study, imaging preoperatively was weight-bearing, and intraoperative assessment was supine. Prior investigation found knee alignment was found to be influenced by weightbearing (Colyn et al. 2023; Zahn et al. 2019; Kato et al. 2023), knee position (Neirynck et al. 2020; Ahrend et al. 2022), and limb rotation (Sun, Yang, Xiao, et al. 2021) which may influence the systematically biased measurement found in our study. An average difference of 1.76 degrees in HKA angle between a double leg stance and supine position uncovered the potential to precipitate prosthesis placement with increased deformity if the preop plan was strictly followed. Knee position impacted on alignment (Neirynck et al. 2020), with approximately half of 545 knees demonstrated alignment changes between flexion and extension and had the magnitude of deformity decrease in flexion for varus and valgus knees. Further, progressive limb loading with weight-bearing has a differential impact on alignment (Zahn et al. 2019), and the authors emphasized obtaining long-leg images under physiologic limb load in full extension. Limb rotation influences measurement +/- 3 degrees as well as weight bearing, flexion of the knee, and weight bearing also play significant roles as described by Sun et. al (Sun, Yang, Xiao, et al. 2021). The authors concluded these 3 dimensional factors should be accounted for during axis measurement, however no set standard exists. Our findings mirror prior assertions that there are significant differences between imaging techniques in TKA, and we similarly emphasize the impact of measurement modality must be accounted for when comparing alignment values (Nam et al. 2016).
We found a systematic bias in the robot measurements in our study, and the magnitude appeared to increase as the magnitude of deformity increased and the knee phenotypes were influenced differently. Similar to our study, coronal alignment measurements on preoperative imaging using EOS scan were strongly positively correlated to coronal alignment on CT (r = 0.927, p = 0.001), though less reliable and deformity magnitude increased (Corbett et al. 2023). It is important to note that the comparison of measurement using correlation has been questioned and has a predilection to lead to misleading findings that are statistically significant (Bland and Altman 1986, 2003). We utilized BA plots and LoA analyses that overcome limitations implicated with correlation analysis. Our data reaffirms that deformity and patient position has a dose-dependent influence on measurement bias (Corbett et al. 2023; Yaffe, Koo, and Stulberg 2008; Willcox et al. 2012).
Decision-making is further complicated by knee phenotype influence on measurements. We found biased measurements differed between varus and valgus knees between preoperative XR and intraoperative robot alignments. Similar findings have previously been reported for pre and postoperative alignment measurement on XR (Hörlesberger et al. 2023). Authors found 46% of patients with preoperative varus alignment shifted to neutral alignment versus 39% of patients with preoperative valgus alignment to neutral alignment, and 39% of patients with varus phenotype remained in a varus alignment versus 58% of patients with preoperative valgus phenotype remained in valgus alignment. An additional consideration is the severity of deformities included, considering the robot data was -17 to +17 degrees. As such, there symmetric bounds of data recorded by the robot were not influenced by clinical exclusion and possibly influenced by hardcoded bounds in the robot. We discussed this possibility with the robot platform teams, and they informed us there is no hardcoded bounds to robot bounds. Similar to the prior articles, we did not have exclusion criteria for deformity severity and the symmetry may be secondary to chance.
We believe we are the first to demonstrate robot systematic measurement bias using a handheld imageless robot. Our study has important limitations to consider. Importantly, navigation and robot systems are not all the same (Mart and Goh 2021; Kayani et al. 2019) and should not be considered representative of all robot systems. Importantly, the dynamic assessments performed by a surgeon are influenced by both the robot measurements and calculations. Nevertheless, we feel this bias has been mitigated in our study since a single surgeon and utilized a standardized workflow. Similar findings have been reported for MAKO robot and navigation systems (Willcox et al. 2012; Glowalla et al. 2023; Han and Lee 2016; Ollivier et al. 2023), which highlights the importance of understanding the idiosyncrasies of each tool assisting the surgeon and decision-making in performing TKA. Second, we do not include patient demographics or postoperative data. Third, rTKA is a complex process with a constellation of variables that my influence the outcome, including the potential differential impact of surgeon, patient, or robot platform variables as they interreact. Consequently, unknown variables likely influenced our data in addition to the variables mentioned above. For example, flexion contracture may influence coronal alignment assessments and no attempt was made to mitigate its influence, especially at the extremes of measure (Sun, Yang, Xiao, et al. 2021). Our main goal is to highlight the discordance of two measurements used in rTKA and not to address aspects of measurement (accuracy and precision) or make claims regarding the merits of radiographic measurements relative to robotic calculations. Notably, we accepted the limitations in our current understanding regarding limb alignment and measurement, which does not meet the assumptions necessary to perform a correlation analysis and employed methods to overcome this knowledge limitations (Courtney et al. 2016; Price et al. 2018; Lombardi, Berend, and Adams 2014). Lastly, our study did not include a comparison of post-operative standing radiographs. We feel the lack of postoperative comparison does not negate the importance of our findings because rTKA is a complex process including preoperative, intraoperative, and postoperative stages that are performed sequentially. Prior studies sought to answer the controversies about alignment philosophies (Gunaratne et al. 2017), technical performance (Aoki 2019), and outcome achievement (Aalen et al. 2015; Andersen et al. 2012), whereas we aimed to investigate the decision-making process bridging the preoperative and interoperative stages that may have downstream ramifications. Nevertheless, we believe our data demonstrated a systematic bias in alignment assessment and believe surgeons should be cognizant of the discordance during their decision-making process. Future studies should investigate if this discordance may impact technical performance and clinical outcomes as well as the potential differential impact on performance and outcomes considering different alignment philosophies.
Conclusions
We found a clinically significant difference in alignment assessment be radiographic measurements and robot calculations. We believe surgeons to be cognizant of this measurement discordance optimal surgical decision-making. Coronal limb alignment measurements should be interpreted with caution, and measurement discordance is a multifactorial problem that has potential to negatively impact decision quality.