Introduction
Total hip arthroplasty (THA) is a well-established and effective procedure aimed at alleviating pain and improving mobility in patients with advanced hip joint osteoarthritis, fractured femoral neck, or avascular necrosis (AVN) of the femoral head (Ferguson et al. 2018). However, limited data exist regarding the technical challenges and outcomes of performing THA in patients with ipsilateral above-knee amputations (AKA) complicated by infected nonunion neck of femur fractures. Younger amputees often have greater functional demands than older patients and require implants to withstand increased stress while carrying a higher risk of revision surgery and dislocation. Performing THA in this population necessitates a meticulous and comprehensive approach because of the unique challenges these cases present (Di Martino et al. 2024). This report details the outcome of THA performed on a limb with an AKA complicated by an infected nonunion neck of femur fracture and AVN of the femoral head.
Case Presentation
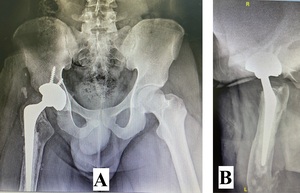
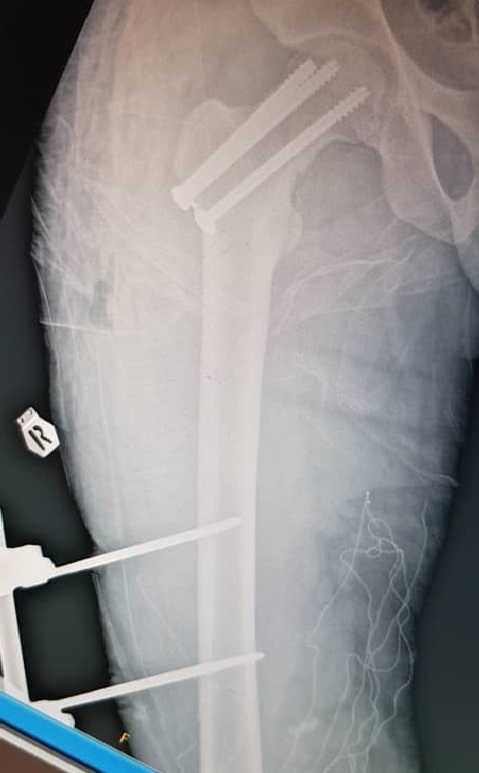
A 22-year-old man presented to our hospital in December 2020 following a motor vehicle accident. The patient had no significant medical, family, or allergy history. He worked in a metal factory and occasionally smoked. The sustained injuries included a closed fracture of the right neck of the femur, an open right supracondylar femur fracture (Gustilo 3C), and an open midshaft fracture of the right tibia (Gustilo 2) (Figures 1, 2, and 3).
Initial management involved screw fixation of the femoral neck, wound debridement of the right thigh, and placement of an external fixator across the right knee (Figures 4 and 5), followed by a one-week course of intravenous cefuroxime. By January 2021, the right leg had become gangrenous and deemed nonviable. Right above-knee amputation (AKA) with adductor myodesis was performed, followed by intravenous cefuroxime for another week.
In May 2021, the patient presented with wound breakdown at the AKA stump and purulent discharge at the femoral neck screw fixation site. Surgical interventions included debridement of the right thigh, right hip arthrotomy and washout, and removal of cannulated screws to treat septic arthritis of the right hip. Laboratory tests showed a CRP of 147 mg/L, and cultures isolated Enterobacter cloacae, which was treated with a six-week course of intravenous Tazocin. Given the advanced stage of femoral head AVN and persistent infection, THA was deemed the most suitable treatment option because alternatives such as core decompression with vascularized bone grafting or derotation osteotomy were not feasible. The patient was scheduled for two-stage revision surgery, and the associated risks and complications, particularly at a young age, were explained to him.
First-Stage Surgery
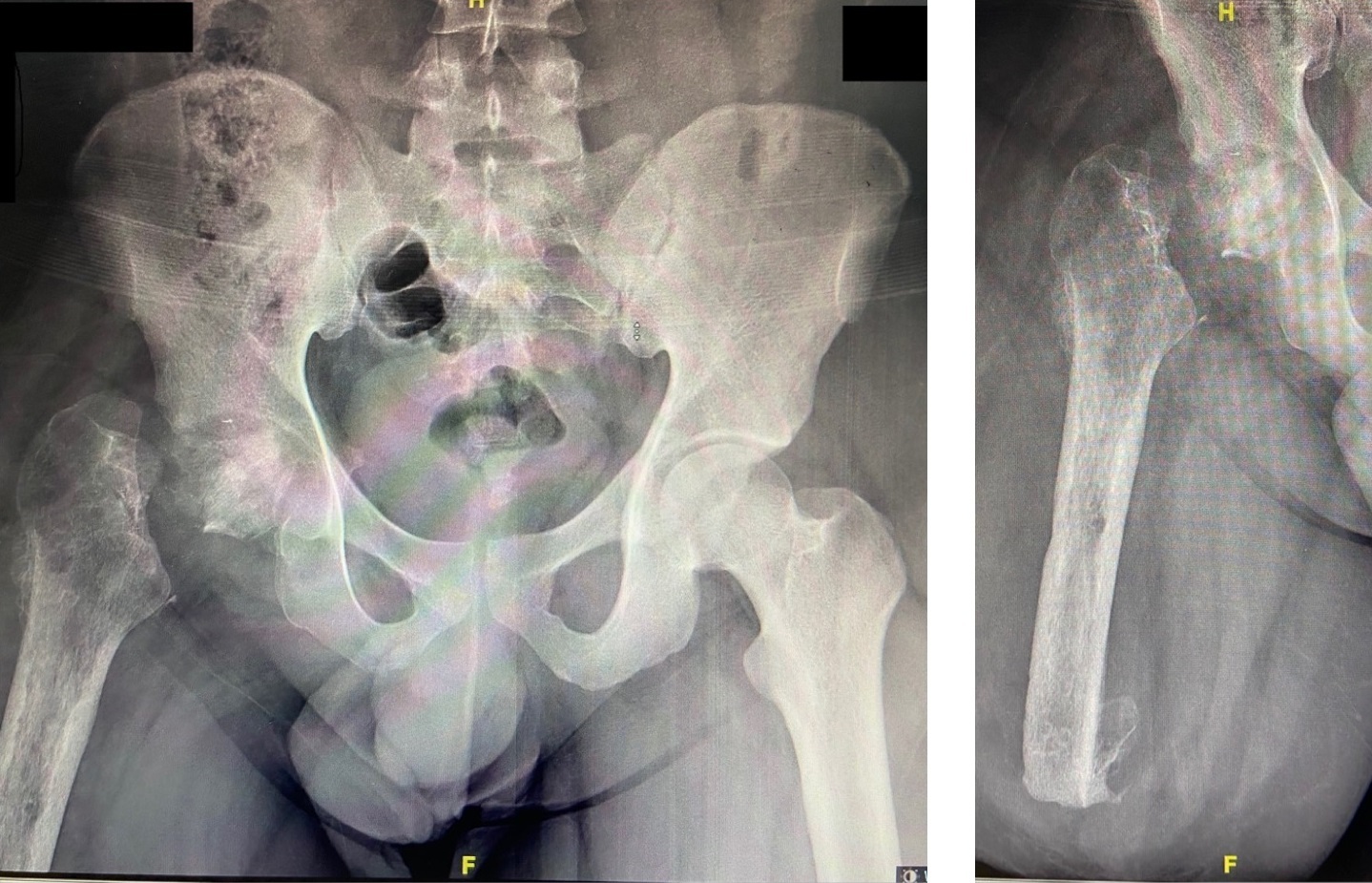
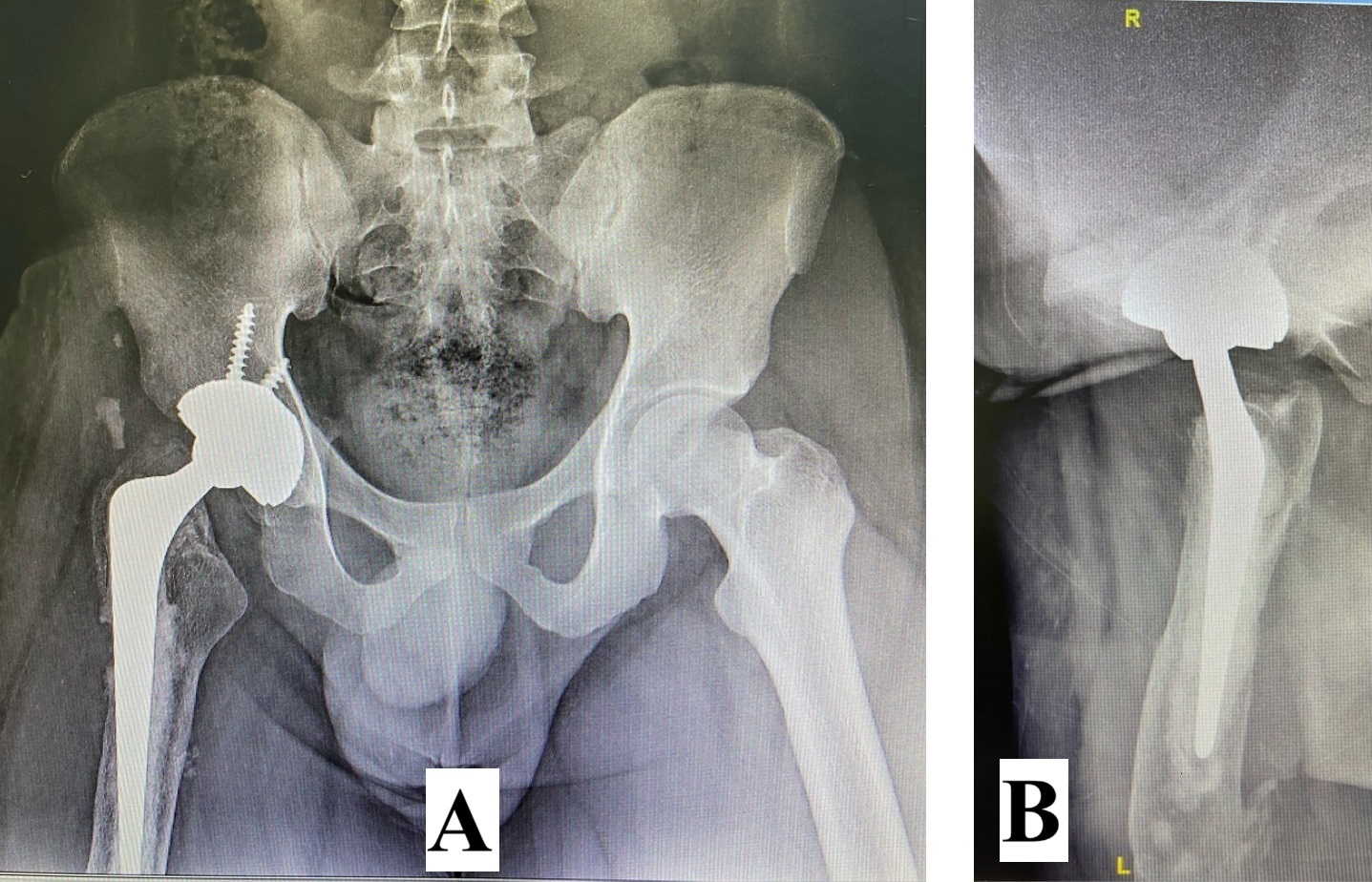
The first-stage revision surgery was performed in December 2021. Preoperative radiographs (Figure 6) revealed an AVN of the right femoral head, nonunion of the femoral neck, and osteopenia of the proximal femur. Surgical procedures included debridement of the AKA stump and removal of the native femoral head, followed by the insertion of an antibiotic-loaded cement spacer. Postoperative cultures again identified Enterobacter cloacae, necessitating a six-week course of intravenous Meropenem. A postoperative radiograph (Figure 7) showed the placement of an articulated antibiotic-loaded cement spacer. By February 2022, after a two-week antibiotic-free period, the patient’s CRP level had decreased to 18.2 mg/L. Hip aspiration performed in June 2022 showed a further decrease in CRP to 10.2 mg/L, with negative cultures.
Second-Stage Surgery
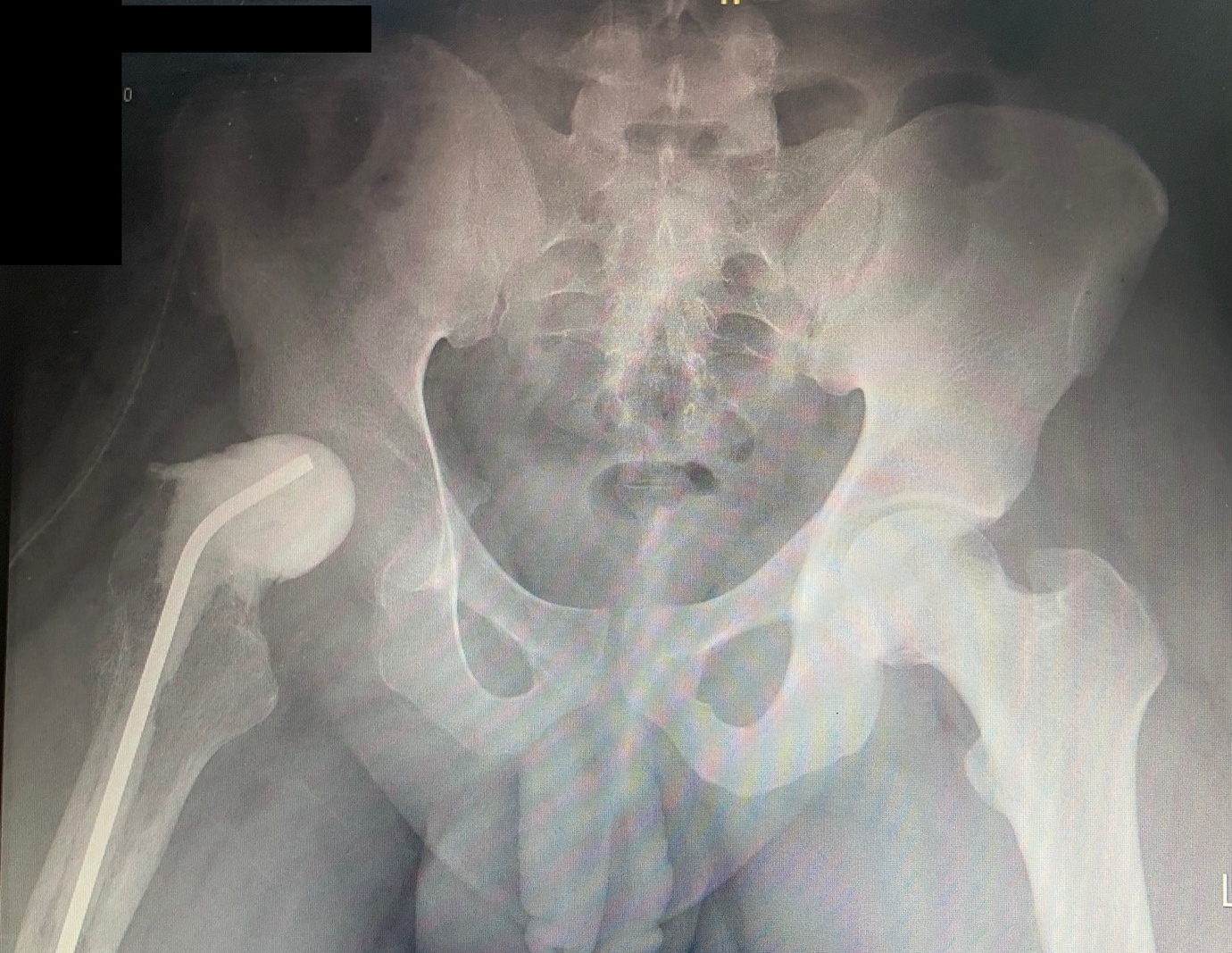
In July 2022, second-stage revision surgery with THA was performed. The intraoperative alpha-defensin test results were negative. The patient was placed in the lateral decubitus position and surgery was performed under combined spinal-epidural anesthesia. A direct lateral approach was used because of existing surgical scars on the lateral aspect of the right hip. The cement spacer was securely fixed and removed using an OSCAR Cement Removal System (DePuy Synthes, Warsaw, IN, USA) and curved osteotomes. The OSCAR system uses high-frequency vibrations to efficiently loosen bone cement, preserve native bone, and optimize surgical outcomes (DePuy Synthes, n.d.).
The femoral canal was thoroughly irrigated with saline before acetabular preparation. A 46-mm uncemented acetabular shell was aligned with the transverse acetabular ligament. Bone-holding forceps were used to clamp the proximal femur, aid femoral stem preparation, and reduce the components. The residual proximal femoral stump measured 220 mm, allowing for the use of a 150-mm cemented femoral stem secured with Simplex P bone cement containing 1 g of tobramycin. The lateral cortex of the femur at the previous screw insertion site was plugged manually during cementation. Component anteversion was determined using the Ranawat test (Ranawat and Maynard 1991), and hip stability was confirmed using the shuck test. A dual-mobility liner was used because of concerns regarding abductor muscle integrity from multiple prior surgeries. The final construct included a 36-mm dual-mobility liner and 22-mm femoral head. Postoperative radiographs (Figure 8) confirmed the appropriate implant placement. Postoperatively, intravenous Cefuroxime was given for three days followed by oral Cefuroxime for three weeks.
The patient’s postoperative course was uneventful. He was fitted with a right transfemoral prosthesis three months post-surgery and followed up for two years, with radiographs at the two-year mark showing stable implants (Figure 9). Table 1 summarizes the injuries, diagnoses, investigations, and treatments of the patients. Although the patient had transitioned from his previous occupation as a metal factory worker to an administrative clerk, he resumed an active lifestyle, performing fitness exercises, riding a motorcycle, and climbing stairs with his prosthesis, albeit with some modifications.
Discussion
THA following an ipsilateral AKA is rare, accounting for only 0.067% of all THAs (Amanatullah, Trousdale, and Sierra 2015). Performing THA in such patients presents unique challenges related to surgical approach, stump manipulation, and femoral component preparation. The principal challenge in this case was management of the underlying hip joint infection. Initial debridement and removal of the femoral neck screws were followed by a six-week course of intravenous antibiotic therapy. Two-stage revision surgery was then performed, which is the gold standard for managing chronic prosthetic joint infections (PJI), with reported infection eradication rates exceeding 90% (Pangaud, Ollivier, and Argenson 2019).
CRP monitoring, negative hip aspiration cultures, and alpha-defensin tests confirmed resolution of infection before the second-stage revision. Extended antibiotic prophylaxis at three weeks postoperatively further reduced the risk of reinfection, consistent with the literature supporting prophylaxis durations of less than one month for successful outcomes (Fang et al. 2021).
Dual-mobility cups were employed to enhance stability, with dislocation rates reported to be significantly lower than those of unipolar cups (Van Beers et al. 2020). Preoperative planning including templating for acetabular component placement and femoral implant selection is critical. In this case, a sufficient proximal femoral stump length allowed for the use of a conventional cemented femoral stem chosen because of osteopenia.
Altered anatomy in AKA patients introduces additional technical challenges, such as a reduced lever arm for dislocation and relocation, limited bone stock, and increased fragility. While Steinmann pins are often used for manipulation in such cases (Diamond et al. 2013; Wagner and Quiroga 2020), this approach was avoided because of severe osteopenia in the trochanteric region. Bone-holding forceps were used to manipulate the femur safely.
Favorable patient outcomes underscore the importance of meticulous infection control, careful preoperative planning, and appropriate implant selection. Currently, the patient is infection-free, ambulates independently, and leads an active lifestyle, highlighting the potential for positive outcomes in similar complex cases.
Conclusion
This case highlights the complexity of performing total hip arthroplasty (THA) in patients with ipsilateral above-knee amputation (AKA) and infected nonunion neck of femoral fractures complicated by avascular necrosis of the femoral head. Successful management requires meticulous preoperative planning, addressing the underlying infections, and leveraging a multidisciplinary approach. The two-stage revision strategy, the use of advanced implant techniques, and tailored physiotherapy play pivotal roles in achieving infection control, implant stability, and functional recovery. Despite significant challenges, the patient regained mobility and improved quality of life, demonstrating that THA can be a viable option in such complex cases when performed with careful consideration of technical nuances and postoperative rehabilitation. This case underscores the importance of individualized treatment plans to overcome the unique surgical and functional obstacles in achieving favorable long-term outcomes.