Billing, Licensing, and Coding
Medicare
There are a few definitions that Medicare uses to describe telemedicine services that one must be aware of.
-
Originating site – location of patient at the time the service is provided (provider must be licensed in this state)
-
Distant site – site where provider is located at the time of the service
-
Synchronous service – remote service performed using live, interactive, real-time communication
-
Asynchronous service –communication between provider and patient is typically via email or text, not in real-time
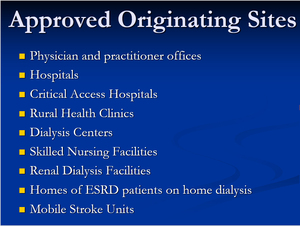
Medicare typically mandates that an eligible beneficiary must be seen at an approved originating site (Figure 1) and by an approved provider (Figure 2). The visits must be real-time, there must be documented patient consent (written preferable, but verbal accepted), and the documentation of the visit must support the level of service that was billed for.
With COVID-19 crisis, many of these rules and regulations have been lifted, but it’s hard to say at this point if they will be re-enforced once the epidemic is under control.
Commercial payors
Depending on the state, coverage for telemedicine services may be none, limited, or broad.
Some states have parity laws that mandate that telemedicine services be reimbursed at similar rates compared to in-person visits. Other key questions to ask individual commercial payors include:
-
Which services are covered and reimbursed?
-
Are there cost-shifting protection measures that prevent payors from shifting excess cost to patients (i.e. charging higher deductible, co-insurance, or co-pays for telemedicine)?
-
What restrictions on acceptable originating sites exist?
-
Is asynchronous telemedicine covered?
-
Are there restrictions on patient type (i.e. can new and established patients be seen virtually)?
Medicaid
All 50 states and DC offer some sort of payment for synchronous telemedicine visits. Currently, 14 states pay for asynchronous telemedicine, 22 states pay for remote patient monitoring, and 23 states have restriction limits for where the originating site can be.
Medical Licensing
One of the basic tenets of telemedicine is that the provider must be licensed in the state where the patient is located at the time the service is provided. The Interstate Medical Licensing Compact has been created as an expedited pathway to licensure for qualified physicians who wish to practice in multiple states if desired. There are currently 29 states that are part of this compact and it is recommended that you contact your individual state licensing board for further information.
Coding
In order to code telemedicine services appropriately, standard current procedural terminology (CPT) codes should be used similar to in-person visits. A place of service code (POS) should be used to identify the location where health related services are provided or received. POS 02 is utilized to refer to a telemedicine visit. Appropriate modifiers should be used to append the CPT code to indicate which type of telemedicine service has been provided. Modifier “95” is used for synchronous telemedicine and modifier “GQ” is used for asynchronous telemedicine.
Hardware
For the purpose of most orthopedic surgeons, any device with a camera and a microphone will suffice. Mobile phones, tablets, laptops, and desktops are all reasonable options. With the initial telemedicine offering, we recommend the utilization of devices that are already available to providers to minimize cost expenditure and administrative burden.
Software
Most existing telemedicine platforms offer much more than what the average orthopedic surgeon requires to do telemedicine visits. It may be helpful, although not necessary, to invest in a platform that can easily integrate into your existing electronic medical record (EMR). Some other important features to look for include a virtual waiting room, text/email notification and scheduling, billing and payment collection capabilities, as well as the ability to screen share. Screen/desktop sharing capability is very important in our specialty as many of these visits will be for image review and surgical discussion.
You want to make sure that the platform you are using is HIPAA-secure. What this means is that the covered entity (hospital or practice) and the software vendor (business associate) have signed a “Business Associate Agreement” (BAA). The BAA outlines the type of protected health information (PHI) that will be transmitted over the platform, the allowable uses and disclosures of the PHI, the measures taken to protect the PHI, and most importantly, the steps that will be taken in case of a PHI breach. During the COVID-19 outbreak, non-HIPPA secure platforms such as Zoom, FaceTime, and Skype will be temporarily permissible, however, it is not recommended to rely on such platforms as a long-term, telemedicine solution.
Practical Matters
Your administrative and clinical assistants will be mostly responsible for making sure that your patients get scheduled and can connect for their telemedicine visits. In addition, you and your assistant are likely going to be the ones to tell your patients that you even offer telemedicine. Ideally, you would have real-time IT support to help with any audiovisual glitches that may arise during a telemedicine visit. However, depending on your practice or hospital infrastructure, you may be “on your own” when it comes to troubleshooting during the visit.
In the beginning, you may want to do these visits early in the morning, after hours, or during your administrative time. With more experience, you can schedule them in conjunction with your traditional clinic. During the visit, you want to make sure that you have a mobile phone, a regular phone, and potentially a laptop or desktop. (Figure 3) It’s helpful to have multiple ways to interact with the patient, both audibly and visually, should your primary hardware device stop working.
Appropriate Patient Selection
We would recommend that you start with established patients that you have previously evaluated and examined, have a good rapport with, and have a relatively simple problem. The easiest visit types to start with are simple post-operative visits as they tend to be very quick and mostly require visual wound evaluation. Other visit types ideal for telemedicine are imaging review, surgical discussion, and range of motion checks.
Conclusion
The key thing to remember is that telemedicine is a tool, just like a reflex hammer or stethoscope is a tool. It should be used in the appropriate clinical situation, by a provider that’s comfortable using it, and for the appropriate patient. Moreover it’s meant to augment and streamline, in-person care, not replace it. Whether it’s to get through the COVID-19 pandemic or to create a long-term digital health solution, you have to do your homework before you implement telemedicine into your existing practice. Make sure to utilize state and federal guidelines, policies, and resources to ensure that you are billing appropriately and are in compliance with the legal and licensing regulations in your state/region. As with any new endeavor, you have to remain patient and flexible, as successful implementation and integration will not happen immediately. We do think telemedicine is a great way to keep our patients, staff, and providers safe during social distancing. More importantly though, we think offering telemedicine is a great way to stay relevant within the evolving healthcare landscape, to provide convenient, high-quality care, and to re-imagine how we deliver care to orthopedic patients.