Introduction
The increase in the geriatric population affects all disciplines in orthopaedics. The burden of hip fractures is well known, with patients having increased morbidity and mortality and decreased return to function (Baer et al. 2019; De Joode et al. 2019; Katsoulis et al. 2017). A common goal to reduce these complications in geriatric patients with fractures is early mobility.
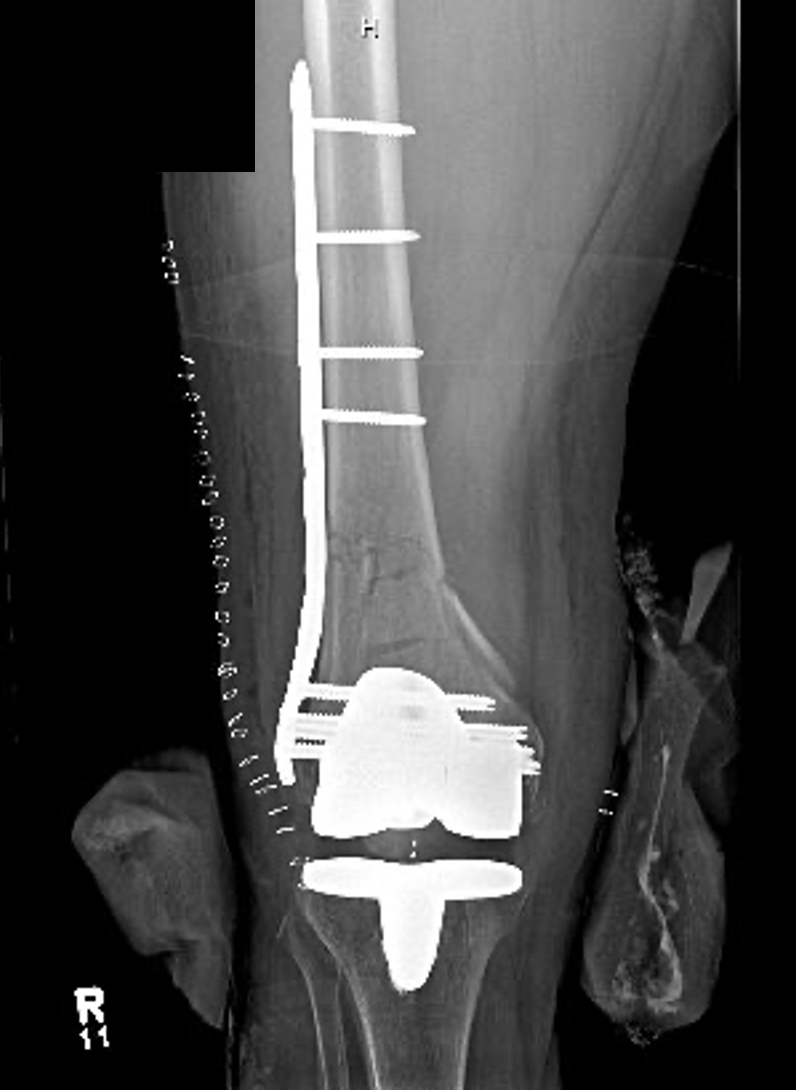
Distal femur fractures are another injury that occur in the geriatric population, often times from a ground level fall/low energy mechanism of injury. Some of the patients may already have a total knee replacement and sustain a periprosthetic fracture. Surgical stabilization of these fractures is the standard of care with acceptable outcomes in the majority of patients (Shulman et al. 2014).
Early mobilization after hip fracture fixation is an accepted practice to minimize morbidities (Koval, Friend, Aharonoff, et al. 1996). In addition, the literature supports early mobilization after tibial shaft and ankle fracture fixation without untoward results (Gross et al. 2016; Dehghan et al. 2016). Early mobilization after distal femur fracture fixation may be beneficial to an elderly patient. The surgeon may be concerned with bone quality and worry about hardware failure. There is only one clinical study we could find on the results of immediate weight bearing after distal femur fracture fixation in a geriatric population with no increase in complication rates (Poole et al. 2017).
The purpose of our study is to determine if early weight bearing in distal femur fractures in the geriatric population maintains fracture reduction and allows earlier return to function. We aimed to complete a pilot prospective cohort comparison study. Our hypothesis is early weight bearing in distal femur fracture in the geriatric population will maintain fracture reduction with no increase in complication rates and similar patient functional outcomes as measured by the Oxford Knee Score.
Methods
We performed a prospective, non-consecutive cohort pilot study (NCT# #02475941) involving 5 Level 1 Trauma Centers. Patients were enrolled at the time of surgical stabilization. The patients were followed at regular intervals clinically and with radiographs until healed. Complications evaluated included infection, loss of fixation and nonunion.
Enrollment Criteria
Patients 64-90 with an OTA 33 type distal femur fracture were eligible for inclusion. Periprosthetic fractures were included. Pathologic fractures were excluded. Patients with additional long bone injuries of upper or lower extremity that would compromise outcome assessment were excluded.
The patients were treated with surgical stabilization. Following surgery, the surgeon decided if patients would be weight bear as tolerated (EWB) or protective/non weight bearing (NWB). Our inclusion criteria ensured patients were independent ambulators prior to the surgery. Physical therapy orders were placed regarding the WB status. EWB were placed as “WBAT with assistive devices” as any geriatric fracture patient with a distal femur fracture who is WBAT would be expected to use assistive devices. Once enrolled, patients were scheduled for clinical follow up visits at 2 and 6 weeks and 3, 6 and 12 months from their injury with a +/- one-week interval. At enrollment and at the 3, 6, and 12 month visits, the Oxford Knee Score Questionnaires were administered, and their scores were calculated. Visual Analog Pain Scores (VAS) were also collected at these visits. Radiographs of the injured extremity were obtained at regular intervals until the fracture was determined to be healed. Additional study driven data was collected.
Fracture healing was determined by treating surgeon with a fracture considered healed if bridging callous present on a single cortex (Strotman et al. 2017).
Nonunion was defined radiographically as failure to achieve bridging callous by six months or evidence of hardware failure.
Treatment Allocation
The treatment allocation in this study was surgeon based. Each participating surgeon treated study subjects by his or her preferred method (Early Weight Bearing or Non /Protected Weight Bearing) with the decision made after the surgical procedure. The operative patients underwent elective plate fixation of their distal femur fracture. The surgical approach, plate brand and size were at the discretion of the surgeon.
Sample Size
The final outcome of this study included healing of the distal femur fracture without hardware failure. A power analysis was completed for 5% difference in healing between the EWB and NWB group. The sample size required to detect a significant difference was 200/group. Based on this information we elected to complete a pilot study over a two-year time interval.
Statistical Analysis
Statistics were performed in SPSS 25.0. Descriptive statistics, as well as Chi-square, Fishers exact, and t-tests, were performed as appropriate. Statistical significance was defined as a p<.05
Results
This was a prospective pilot study involving 5 Level 1 Trauma Centers. The enrollment period was from January 2016 to October 2018.
Demographics
There were 46 patients with an average age 75 (range: 64-90). Thirty-three patients (72%) were female and 13 (28%) were male. Forty (89%) patients were Caucasian and 5 were African American (11%). One patient declined to answer. Eleven patients (24%) were in the EWB group. There were 14/46 (30%) obese patients with a BMI> 30. However 13/14 were in the NWB group, accounting for a potential confounding variable. There were 4 patients with diabetes. All were in the NWB group. Twenty patients were smokers. There was no statistical significance in demograpghics between the groups. (Table 1) The follow up was 37 patients (80%) at 12 weeks; 28 patients (61%) at 6 months and 19 patients (41%) at 12 months.
Injury Characteristics
There were 37 33A, 2 33 B and 7 33C fractures. Forty-five percent (5/11) in the EWB group and fifty-one percent (18/35) in NWB group had periprosthetic fractures (P=0.73). (Table 2) Ninety-six percent (44/46 patients) were injured in low energy ground level falls. Two patients were high energy (falls > 4 feet) with one patient in each group (EWB and NWB).
Surgical Details
Prior to definitive fixation, 2/46 (4.3%) were treated in an external fixator, 40/46 (87%) in knee immobilizer and 3/46 (6.5%) in a splint and 1 in traction. On average, surgery was performed 2.09 days from injury (SD1.86, range 0-11days). Ninety-one percent (42/46) were approached through a lateral incision. The remainder had surgical stabilization through an anterior approach (9%). The majority of patients (42) were treated with a pre-contoured locking plate with the distal construct locked. The use of locking and non-locking screws varied. However, the majority of patients (36) were treated with all non-locking screws above the fracture or a hybrid construct of one or two locking screws above the fracture. Ten patients were treated with 3 or more locking screws above the fracture. In three patients, there were additional plates used for fracture stabilization (2 NWB, 1 EWB).
Union rates
Radiographic union was determined by treating physician regarding presence of bridging callous. At week six 40/46 (87%) were deemed healed radiographically. There were two hardware failures (one at 6 weeks and one at 12 weeks), both in the NWB group. The remaining 4 fractures were all deemed healed at 12 weeks.
In the NWB group, there were 2 hardware failures. In the EWB group, there were no hardware failures or additional surgeries. While the group was small, there were no hardware failures in the EWB group. However, since the weight-bearing status was determined by the treating physician, there was a tendency to treat obese patients in the NWB group (9% of EWB were considered obese where 37% of NWB were obese). In the NWB, 1 failure was obese, 1 was not.
Outcome Measures
The VAS scores were reported as < 5 in 44/46 patients at 6 and 12 weeks. 13 patients reported no pain (VAS=0) at six and twelve weeks. Narcotic use is of concern in orthopaedics, especially in the elderly. In our patient study, 22/46 (48%) never used narcotic pain medication. 19/46 (41%) used narcotics for less than one week. At 12 weeks, only one patient reported narcotic use with a healed fracture and no complications and reported VAS score of 10. There was no difference between the groups.
Oxford scores at baseline ranged from 16-48; at week 6 was 5-44 and at week 12 was 5-43. There were no significant differences between the groups in any variables. (Table 3)
Complications
There were two hardware failures (one at 6 weeks and one at 12 weeks), both in the NWB group. Both patients had stainless steel plates. One of these patients did not desire additional surgery. This patient had 3 non-locking and one locking screw above the fracture. The other complication occurred in a patient treated with all locking screws above the fracture and underwent revision surgery.
In our pilot study, we had a 6.5% mortality rate. Only 1 patient of these patients was operated on after two days (at 4 days from injury). Two patients died at 12 weeks, with the third death reported at one year from unknown causes. The first patient died from unknown causes. The second patient who died was seen and evaluated for chest pain, sent home and died of a cardiac complication. All three patients who died had the commonality of being in the NWB group, were obese and had diabetes mellitus. There were no deaths in the EWB group. This difference was not significant, p=.4.
Discussion
Early mobilization after fracture fixation is thought to be beneficial. Previously, many types of lower extremity fractures were kept non-weight bearing, often due to surgeon concerns regarding implant or fixation failure.
Early mobilization in the elderly after hip fractures has been accepted for several years (Koval, Friend, Aharonoff, et al. 1996). However, early mobilization after fractures of the distal femur remains controversial. Granata, et al. evaluated the biomechanics of immediate weight bearing of distal femur fractures treated with locked plate fixation in cadavers (Granata et al. 2012). They found that the fatigue limit of the locked plate constructs was 1.9 times body weight for an average 70-kilogram patient over a simulated 10-week postoperative course. Although this study could not fully support immediate weight bearing due to the fact that femoral loads during gait have been estimated to be around 2 times body weight, it demonstrated adequate hardware fixation with weight bearing. While this cadaveric study suggested hardware fixation could be maintained with weight bearing, there is little clinical data to support this.
Nichol. et. al. evaluated immediate early weight bearing in a cohort of patients treated with a distal femoral locking plate over a 5-year period (Poole et al. 2017). In their study of 127 patients who had an average age of 73, 107 were allowed immediate weight bearing. The reoperation rate was only 3% in this group of predominantly female, elderly patients. Our results found no increased complications with weight bearing after distal femur fracture fixation, but we found there most likely was selection bias in that 13/14 patients considered obese, were placed in the NWB group. A prospective, randomized study could eliminate that bias in determining EWB.
Nichol et al also had a large percentage of extraarticular fractures (67%) and also periprosthetic fractures (56%) (Poole et al. 2017). There was a limited number of intraarticular fractures in both his and our study. We also had 80% extraarticular fractures. With the elderly patients, this is not uncommon. While Nichols study included patients ages 16-101, our study was exclusive to elderly patients. The fracture type that has not been adequately evaluated is intraarticular distal femur fractures. Our numbers were similar to that study regarding intraarticular fractures (15% vs. 13%). The low percentage in both studies may be a function of fracture type more likely to occur in the elderly. Patients with intraarticular fractures were permitted EWB in both studies, but the small numbers warrant caution in application of EWB for intraarticular fractures.
A prospective cohort was used because weight bearing as tolerated has been proven in the hip, whereas the distal femur has been treated with protected weight bearing. With little data on the safety of immediate weightbearing, we felt we would have significant problems in accruing patients and collaborators into this study with a pure randomized protocol. In addition, the patient might be reluctant to participate in a randomized study where the treatment choices are between immediate weight bearing and delayed weight bearing. A prospective, pilot observational cohort would allow surgeons to enroll patients in this study feeling that they are getting the treatment their treating surgeon feels is best for them after performing the definitive surgery. Our pilot results contribute to the body of knowledge supporting early weight bearing and provide a model for development of future studies.
The surgeon does control hardware stiffness in periarticular plates with selection of diaphyseal screw fixation. Our study left screw construct up to the operating surgeon. In a retrospective review of distal femur fractures by Crist et al, those patients with all proximal locking screws were found to be 2.9 X more likely to lead to nonunion (Harvin et al. 2017). With only two failures in our study, the numbers are too small to draw new conclusions, but it is important the surgeon consider and construct stiffness as appropriate.
Another factor contributing to plate failure is implant material. In the literature stainless steel plates have been found to withstand more cycles to failure and tolerate higher loads (Kandemir et al. 2017). In our study, the two patients with plate failure had stainless steel plates. However, Vrahas et al found a 41% nonunion rate with stainless steel plate and only a 10% nonunion rate with titanium plates (Rodriguez et al. 2016). No conclusions can be made from our study numbers, but awareness of factors affecting healing and failure important to keep in mind with fixation of these fractures in the elderly.
There is limited epidemiological data regarding the occurrence of distal femur fractures in the aging population. A recent study from Denmark, found the occurrence to sharply increase after the age of 60 and is more common in females (Elsoe, Ceccotti, and Larsen 2018). To be included in our study, one had to be 64 or older and we did find the majority of patients were females. Weber et al evaluated 283 patients retrospectively with distal femur fractures and an average age of 76 (Myers et al. 2018). The one-year mortality rate was 13.4% with an increase for patients who had surgical fixation more than 2 days after admission at all time periods evaluated (30 days to one year). A confounding variable was the Charlson Comormidity Index (CCI) was lower in those operated on within the first 48 hours. In our pilot study, we had a 6.5% mortality rate. All 3 patients were in the NWB group.
One patient was operated on after two days (at 4 days from injury). There were no deaths in the EWB group. It is hard to draw conclusions from this small sample size. What we noted is all three patients who died were obese and had diabetes.
This is in stark contrast to the retrospective study by Tarkin et al in 2016 who painted a dismal picture for elderly distal femur fracture patients with a 25% mortality rate and 38% complication rate (Moloney et al. 2016). Also predictive of mortality in their study was age and a higher Charlson Comorbidity Index (CCI). They also had a 24% nonunion rate in the 99 patients with one year follow up. A consistent factor amongst this and the Weber et al study was surgical fixation in less than 48 hours leads to decreased mortality. Our average time to fixation was 2 days. Factors which cannot be controlled definitely contribute to outcome, but surgeons should control what factors they can to minimize complications.
Limitations
In the geriatric population, those patients allowed to advance to early weight bearing have potential for selection bias. Our inclusion criteria indicated the patients had to be household community ambulators at baseline. The surgeons may have selectively advanced patients who had high levels of preoperative activities of daily living that including active physical activity.
Full compliance to EWB or NWB protocol is unknown in both groups. We assume similar levels of complications if both are non-compliant. We do not believe the failures in the NWB group were related to non-compliance.This study (similar to other published studies on early weight bearing) had no definitive measure (sensors for example) of patient compliance with their weight bearing protocol.
Another limitation of possible selection bias is 13/14 obese patients were in the NWB group. However, a review of literature and early weight bearing did not differentiate by body weight/BMI and failure of fixation in the literature cannot be attributed solely to BMI. A randomized study could eliminate this concern.
Follow up is a known limitation of trauma patients, even in the geriatric population. Our main outcome measure was hardware failure/nonunion. All fractures were judged as healed by the treating surgeon at 12 weeks with the exception of the two plate failures. Six months is adequate for detection of plate failure in a healed fracture, so we believe the results are applicable clinically.
Conclusion
Our results demonstrate EWB can be safely done in a small cohort study for geriatric distal femur fractures. Early mobilization has the advantage of a more rapid return to function for the geriatric patient with minimal complications. Additional research with the possibility of a randomized controlled clinical trial could be useful in geriatric distal femur population.
Conflicts of Interest and Source of Funding: The authors report no conflicts related to the topic of this study. Funding was received from the Foundation for Orthopaedic Trauma.
Acknowledgements: Maria Manson, BS; Nancy Hassell BSMT; Christine Townsend, BS; Irshad Shakir, MD
NCT Registration: #02475941
Corresponding Author:
Lisa K. Cannada, MD
Phone: 972-922-6390
Email: cannada.lisa@gmail.com