Background
Beginning an orthopedic surgery residency can be a daunting challenge for a graduating medical student. It requires intense training across multiple disciplines and dedication to long hours of learning complex surgical procedures. Successful orthopedic training includes mastering the orthopedic principles while developing a high level of surgical skills. Developing these skills early in residency can be challenging, as junior residents have significant out-of-the-operating-room responsibilities, and the working hour restriction may limit their operative exposure. When junior residents are able to operate, their involvement in each case is determined by the attending surgeon. Surgeons are often reimbursed on a per-case basis, which incentivizes efficiency in the operating room, often leading to less in-case involvement for junior residents, who are still learning to be efficient. To combat this, most training programs use a combination of educational videos, sawbone/cadavers labs, and physical stand-alone simulators for junior residents to hone their skills. While some programs have successfully incorporated these modalities into their training, they can be expensive, have limited clinical applications, limited accessibility, and can be labor-intensive to keep up to date. Furthermore, these modalities do not fully expose the junior resident to the entire operative experience, limiting their opportunity to develop surgical efficiency outside of the operating room. There is a need to improve the education approach for junior orthopedic residents, and several orthopedic residency programs have begun exploring the possibility of using immersive virtual reality to augment traditional orthopedic surgical training and attempting to maximize the opportunity for each individual resident.
Immersive Virtual Reality (iVR) technology is revolutionizing medical education and surgical training and can potentially mitigate some of the challenges associated with traditional surgical training (Hasan et al. 2022). This modality allows for a purposeful and deliberate approach to education and yields a superior approach to gaining mastery of a topic (Ericsson 2004). Multiple studies have demonstrated the impact iVR can have on resident education and understanding some of the nuances of each technical approach (Sheehan et al. 2021; Feeley et al. 2021; Lohre, Bois, Athwal, et al. 2020). With its immersive capabilities and realistic simulations, iVR offers orthopedic surgery residents unprecedented opportunities to enhance their skills in a safe, low-risk, and controlled environment (Feeley et al. 2021). iVR-based training has been shown to improve residents’ surgical proficiency, confidence, and overall performance while enhancing surgical skill acquisition (Lohre, Bois, Athwal, et al. 2020; Nousiainen et al. 2018). This technology allows the resident to make meaningful errors during critical portions of the case without any risk to the patient. Focusing on skill acquisition in this environment gives the resident an understanding of why procedures are done in specific steps and may help reduce the learning curve of an individual. Surgical training programs have begun examining iVR in their education, finding that it led to superior learning efficiency, increased knowledge retention, and decreased operative times (Lohre, Bois, Pollock, et al. 2020). As iVR continues to evolve, its integration into orthopedic residency programs has the potential to positively impact the next generation of orthopedic surgeons by equipping them with the necessary skills and confidence to excel earlier in their training. This report aims to give real examples of how iVR training can be used to enhance the skills of a first-year orthopedic surgery resident.
Immersive Virtual Reality Experience
A first-year orthopedic surgery resident participated in a comprehensive iVR training program that was integrated into the education curriculum and also coupled with real-time cases in the operating room. The resident used the PrecisionOS ™ iVR system. For each case, the resident had the opportunity to use iVR simulations to learn the principles of surgery, several technical details and surgical workflow of the case prior to entering into the operating room. The modules on this platform included basic anatomy, surgical approaches, arthroscopy, arthroplasty, and fracture cases across all orthopedic disciplines.
In the first month of residency, every weekday, there was protected time specifically for iVR training in order to go through all the modules in the system. There was an attending physician present for each module, either participating in virtual reality through a separate headset in collaboration mode (figure 1) or watching a live screen casting of the virtual procedure. In this setting, the attending was able to provide feedback in real-time in a controlled environment. After the first month, the resident dedicated a minimum of thirty minutes per week of training on the iVR System.
Immersive Virtual Reality Education
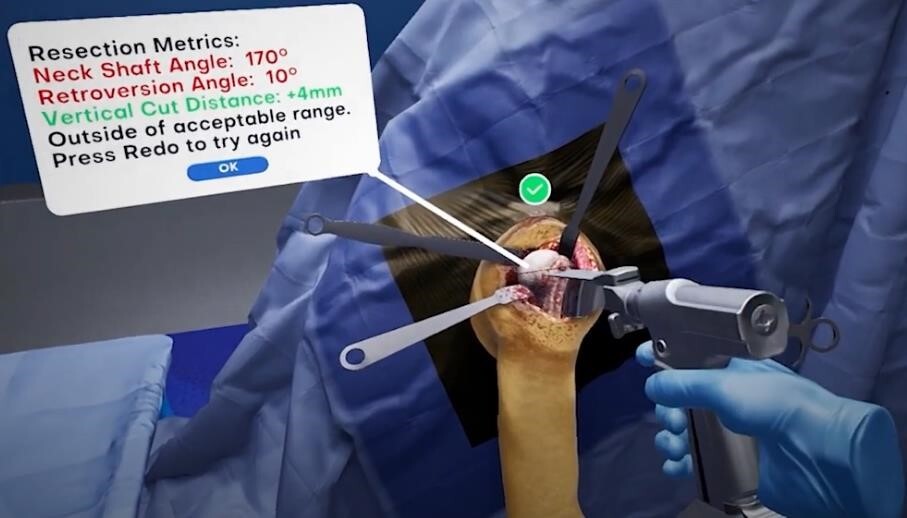
The system actively teaches each procedure and gives immediate feedback throughout the modules. If the resident made an error or skipped a step, the software would not move forward until those parameters were corrected (figure 2). The system analyzes and gives users a visual display of their metrics from each individual module. It allows users to measure and monitor their training progress. Residents are able to hone their surgical skills without any risk of their mistakes causing harm to patients. The virtual environment accurately recreates the real-world operating room (OR), which allows the user to practice the three-dimensional spatial awareness needed during surgery. It even allows the user to position and take X-rays using the virtual C-arm throughout the case without radiation exposure.
The virtual reality education software has modules that mirror, and are linked to the Accreditation Council for Graduate Medical Education (ACGME) milestones, for orthopedic surgery. The residency program leadership is able to track and monitor each resident’s performance on specific modules to ensure they are progressing appropriately.
iVR for Case Preparation
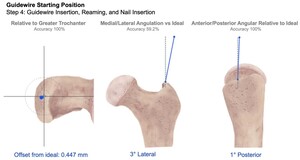
Intertrochanteric femur fractures are one of the most common orthopedic injuries, accounting for approximately 50% of hip fractures, with an average of 150,000 per year in the United States (Karadsheh, Tarazona, and Lambers 2023). While preparing for an intertrochanteric femur fracture case, the resident would utilize the iVR platform to practice the case until a level of proficiency and comfortability was developed. In these simulations, the resident received instant feedback on every step through the analytics dashboard (figure 3). Attending surgeons were able to walk through the case in the virtual reality environment with the resident as well as see their results after the case was completed. This allowed the attending surgeons to have a greater trust of the first-year knowledge of the case and allowed for appropriate graduated autonomy during the case.
Discussion
Utilizing iVR training in addition to the traditional orthopedic surgery curriculum allows the resident to get real-time feedback, learn the anatomy, and master several principles of surgical skills prior to the operating room. The iVR training, coupled with real cases and attending feedback, has the potential to produce more competent, skilled orthopedic surgeons by accelerating their training outside the OR so they can maximize education with an expert mentor in the OR. . A key advantage of iVR to other operative simulations is how closely it mimics the operating room setup and the accuracy of the individual modules to the real-life procedure.
The integration of consistent iVR training into this first-year orthopedic surgery resident’s education significantly enhances their surgical skills, confidence, and trust from attendings. The repetitive nature of iVR, combined with constant feedback, allowed the resident to refine his technical skills, and with time, the steps became muscle memory. The resident observed a noticeable improvement in overall efficiency and proficiency in performing orthopedic procedures.
From the attending’s standpoint, the guided preoperative preparation increased their confidence and trust in the resident allowing for increased autonomy when it came time to do the real case. The attendings preferred to give real-time instruction and feedback in the iVR module, making active changes and modifications prior to stepping foot in the operating room. If a mistake was made in the iVR space, it was very easy to reset the step and practice until it was perfect, whereas if this type of mistake was made in the real operating room, it could lead to devastating results for the patient. The attendings also reported improved surgical efficiency after the training, as the first-year resident was able to anticipate the steps of the procedure, which led to a significantly smoother and shorter operative time.
This article is not without limitations as it is an editorial describing one resident’s experience with iVR and how it was incorporated into medical training. Follow-up research studies with large cohorts and long-term results are necessary to further evaluate iVR for medical training. Another limitation is the availability of learning modules on the VR software. However, the companies are in the process of expanding the number of educational modules available.
Conclusion
Immersive Virtual Reality (iVR) clearly benefits a junior orthopedic surgery resident, as it improves surgical efficiency, increases surgical skills, and establishes a stronger working relationship with the attending surgeons. iVR training represents a valuable adjunct to traditional orthopedic surgery education by providing a safe environment to learn individual procedures and expand a resident’s surgical skills. As technological advancements continue to be incorporated into orthopedic residency education, iVR will continue to play an increasingly integral role.