INTRODUCTION
Chondroblastomas are a type of rare bony neoplasm, constituting less than 1% of all bone tumours (Chen and Difrancesco 2017). It consists of chondroblasts, immature cartilage producing cells, and it largely affects those in the second decade of life. The most common reported symptom is pain, with associated symptoms varying depending on the location (Garin and Wang 2008). In the case of chondroblastomas, common locations include the epiphysis of long bones such as the tibia, humerus, or femur (Kurt 1989). Osteochondral lesions, also known as osteochondritis dissecans, are reactive, benign, change of cartilage or subchondral bone commonly in response to repetitive microtraumas, though the exact etiologies are unknown. It occurs commonly in juveniles, with adult cases suspected to be due to unresolved juvenile lesions (Chau et al. 2021). Symptoms vary, but is commonly some form of mechanical pain with intermittent stiffness and swelling (Bruns, Werner, and Habermann 2018).
With respect to the long term progression of untreated chondroblastomas, it can exhibit local aggressiveness despite its benign nature, leading to significant joint pain, effusion, and functional impairment. Though rare, symptoms can progress to joint destruction, permanent deformities, and chronic bone weakening (Bhatti, Mourougayan, and Harshvardhan 2024). Aside from local aggression, chondroblastomas can exhibit metastatic features systemically, though this is a rare complication of untreated or improperly treated chondroblastomas (Samargandi et al. 2024). Hence, despite the benign nature of chondroblastomas, the choice to intervene in this particular case was done to preserve the joint and halt tumour progression, especially given that the patient is a highly active individual.
CASE REPORT
An 18-year-old Malay gentleman came to the clinic complaining of left knee pain with rest and analgesia providing limited symptomatic relief. He had a history of an anterior cruciate ligament (ACL) and meniscal tear secondary to a soccer injury about two years prior. Following which, an arthroscopic reconstruction of the ACL and repair of the meniscus was performed. Previous visits to the doctor saw complaints revolving entirely around the right knee, from its initial trauma, subsequent surgical repair, and post-operative recovery with no issues with the left knee prior to this complaint.
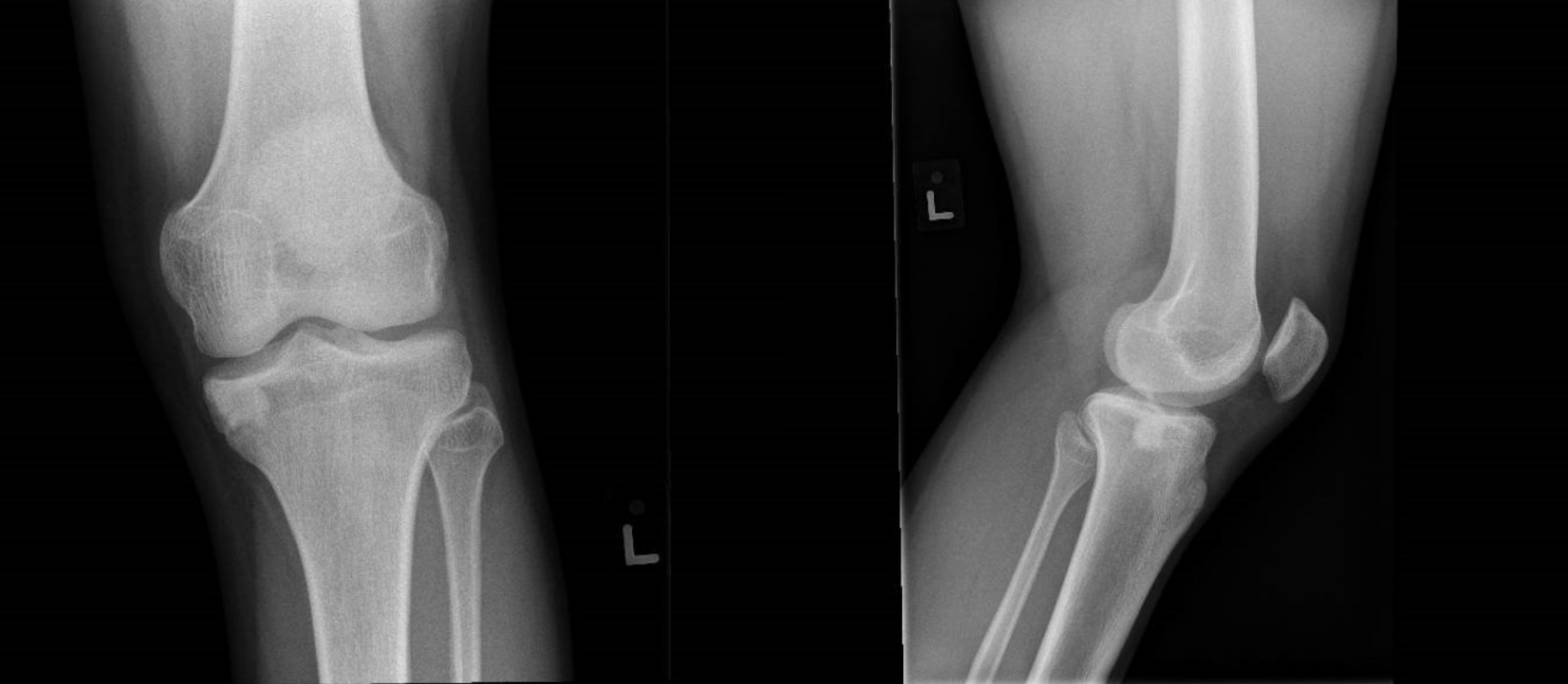
On examination, the only notable finding was severe tenderness along the left medial joint line. A left knee radiograph and magnetic resonance imaging (MRI) were ordered.
An MRI of the left knee was performed using fast spin echo techniques. A hyperintense lesion measuring 1.2 cm × 0.7 cm × 0.9 cm along the cartilage of the medial tibial plateau was identified, which was associated with significant marrow edema extending to the tibial eminence (Fig. 1). The tibial lesion was not well appreciated on the radiograph performed. Such a finding would point toward an undefined osteochondral lesion based on its site and characteristics, and given the profile of an avid soccer player, physical findings, and considering more epidemiologically common conditions, the diagnosis of a benign osteochondral lesion was made.
A therapeutic left knee arthroscopy and microfracture with retrograde drilling was performed. Intraoperatively, a 1 by 1 cm softened segment of cartilage was found on the posteromedial aspect of the tibial plateau, supporting the diagnosis of a medial osteochondral lesion on the left tibia.
Post-operatively, the recovery seemed to go as planned. The patient was fitted in a Breg® Knee Brace (Breg, Inc., Carlsbad, CA, USA) and advised to maintain partial weight bearing with crutches, while also adhering to a range of motion restriction 0 - 90 degrees for 1 month. During a follow-up 1 month post-operatively, there was significant improvement in pain and full range of motion with slight knee discomfort on weight bearing activities. Mild quadriceps atrophy was also noted and the patient was advised to continue physiotherapy for strengthening while avoiding any overly strenuous activity or sports. When reviewed 2 months later, an x-ray of the left knee showed a persistence (Fig 2), but a seeming reduction in size of the tibial lesion.
After another 2 or 3 months, or a total of a year and a half since the first presentation of left sided symptoms, the patient returned with similar symptoms of left medial knee pain that was reportedly worse than before, in the absence of any trauma. There was full range of motion with significant medial joint line tenderness without any swelling on physical examination. This prompted the consulting surgeon to opt for an MRI to re-evaluate the condition of the left knee, and the previously suspected benign lesion.
The MRI taken would reveal the medial tibial lesion previously found to have increased in size, now to 1.3 cm by 1.0 cm by 0.9 cm (Fig 3). Other structures in the knee appeared intact with a similar amount of marrow edema to the previous result. Given that the patient had undergone a therapeutic arthroscopy with microfracture surgery just months prior, expected signs were regression of the lesion with signs of good bone healing, accompanied by an improvement in symptoms. However, the increasing size of the lesion and persistent pain was labelled as highly suspicious, with the consideration of other diagnoses for the initially confirmed osteochondral injury. The patient was referred to a musculoskeletal oncologist, who, taking into account the non-aggressive nature of the lesion seen on the radiograph, as well as its location and the patient’s history, concluded that the lesion was likely a chondroblastoma. Extensive perilesional edema was noted on MRI, appearing as bright T2 signals surrounding the lesion, which did not enhance significantly on T1 imaging.
An intralesional resection was performed through a minimal incision to limit contamination, incorporating an open bone biopsy using a medial trapdoor technique (hinging on the insertion of the pes anserinus and periosteum to promote quicker healing) (Sakamoto, Noguchi, and Matsuda 2022; Wong and Mahadev 2021). The procedure involved curettage, followed by the application of dehydrogenated alcohol as a local adjuvant, and the cavity was filled with nitrogen bone chips and HydroSet® (Stryker Portage, MI, USA) , a bone substitute, for cementing. Intraoperatively, the lesion had sclerotic margins and consisted of cartilaginous content mixed with cancellous bone, without any soft tissue component. A histological examination of the resected sample was suggestive of a chondroblastoma.
Postoperatively the patient was kept on analgesia and physiotherapy with watchful monitoring for recurrence of the chondroblastoma (Fig 4). He remained non-weight bearing for 6 weeks, followed by partial weight bearing for an additional 4 weeks, and then progressed to weightbearing as tolerated to ensure optimal healing of the bone window and subchondral bone. More details of his postoperative timeline are elaborated on below. Additionally, he was placed on a knee brace, and advised to ambulate with a crutch. Significant modifications were made to the patient’s lifestyle to reduce chances of future fractures associated with the lesion at the left tibia, namely the adjustment of his military service requirements.
Post-operatively, the patient was placed on a Breg® Knee Brace (Breg, Inc., Carlsbad, CA, USA) and advised to ambulate in a crutch without any strenuous activity.
At the 6 week follow-up appointment, the patient was recovering well and complained of mild throbbing pain over the wound site. There was no sharp pain or swelling over the incision site. The patient was able to ambulate with a steady gait using a crutch and his brace, without returning to any strenuous activity.
At the 2 month follow-up appointment, there was an overall improvement in symptoms. The patient was able to resume walking without the use of the crutch, had taken off the brace, and complained of mild discomfort.
At the 5 month follow-up appointment, the patient was able to begin jogging but had not yet returned to his sport of soccer. There were complaints of joint tenderness only after his jogging and was advised to reduce his physical activity.
At the 8 month follow-up appointment, the patient had begun to return to playing soccer and had no notable complaints or issues with ambulation. Range of motion was full, and there was no locking or tenderness.
At the 3 year follow-up appointment, there were no new complaints or symptoms, and was advised to monitor for metastatic symptoms such as coughing or hemoptysis.
Plain radiographs performed during a follow up at the clinic 3 years post operation showed a stable focal sclerosis with a rim of lucency due to the effect of cryoablation. This lucency can be confused with recurrence, but serial plain radiographs have shown no progression thus excluding recurrence in our case (Fig 5). The patient had returned also to competitive soccer and remained symptom-free.
DISCUSSION
This particular case highlights several points of interest. The first involves the diagnostic challenge presented by the similarities between chondroblastomas and osteochondral lesions. Secondly, this case also examines the management methods employed for this incidence of a chondroblastoma.
Both lesions exhibit a relatively overlapping epidemiology, with a peak incidence in the second decade of life and being found more commonly in males as compared to females (Bruns, Werner, and Habermann 2018). Most notably, chondroblastomas are extremely rare, making up less than 1% of all bone tumours, both in Singapore and around the world, making them rarely encountered, and highly unexpected, in clinical practice (Chen and Difrancesco 2017).
Both lesions also present with markedly similar features, which is a challenge shared amongst many other bony lesions (Harris 1936). Non-specific symptoms such as pain, stiffness, and swelling, may be present, but not always reported, furthermore confounded by patient tolerance and analgesia use. Additionally, patient history often fails to offer added clarity, as chondroblastomas typically lack any history of injury, whereas osteochondral lesions are often associated with repetitive trauma over time (Bruns, Werner, and Habermann 2018; Yang et al. 2012). Notably in this case, the patient did indeed have a history of repetitive sports traumas, and his only complaint on admission being pain. Given such a history, the diagnosis of an osteochondral injury might be initially favoured over a bony neoplasm, especially when mechanical stressors are thought to be large contributory factors to osteochondral injuries, particularly during activities such as pivoting or running (Bruns, Werner, and Habermann 2018).
Above and beyond history and physical examination, imaging is crucial in modern medicine for accurately diagnosing musculoskeletal conditions. Radiographs and MRIs are foundational in the assessment of these lesions. However, the differentiation between chondroblastomas and osteochondral lesions remains challenging due to overlapping imaging features.
When considering plain radiographs, chondroblastomas are typically characterised as well-circumscribed, lytic lesions with a sclerotic rim, often with central calcifications indicative of chondroid matrix mineralisation (Grimm et al. 2017). Osteochondral lesions may initially present with subtle radiographic signs such as light radiolucencies and/or epiphyseal contour abnormalities. As both progress, they may exhibit a more defined border with better defined features - but in early stages, both lesions can appear similarly on radiographs, making them easily confused (Chau et al. 2021).
For many orthopaedic conditions, Magnetic Resonance Imaging is considered the ‘gold standard’ for evaluating bony lesions with soft tissue involvement. For chondroblastomas, key findings include a hypointense sclerotic rim with associated marrow and soft tissue edema visualised best as bright T2 signal, contrasted by low enhancement on T1 imaging surrounding the lesion (Grimm et al. 2017; Oxtoby and Davies 1996). T2-weighted imaging is particularly useful in accentuating heterogeneous signal intensities often due to inconsistencies in the lesion’s contents, such as calcifications or chondroid matrix variations (Grimm et al. 2017). Co-occurrence of other factors like aneurysmal bone cysts can also further complicate the radiological appearance (Grimm et al. 2017). Similarly, MRI findings for osteochondral lesions are variable, having inconsistent signal intensities, though edema on T2-weighted images is a common feature - similar to that seen in chondroblastomas (Kijowski and De Smet 2005). Given the overlapping imaging characteristics, differentiating these lesions based solely on MRI can be challenging.
In this case, the presentation, imaging, and symptomatology seemed to be more suggestive of a non-neoplastic epiphyseal lesion. When evaluating a benign mass, differential diagnoses would also consider more common lesions such as aneurysmal bone cysts, which is a non-neoplastic, lytic lesion typically commonly found in individuals under twenty and accounts for roughly 9.1% of bony masses detected radiologically (Hakim et al. 2015). Another more common differential is a giant cell tumour, which is typically located in the epiphysis of long bones, especially around the knee, and comprises approximately 20% of all benign bone tumours (Hakim et al. 2015). These conditions serve as diagnostic confounders and highlight the importance of careful differential consideration by clinicians.
When examining the management employed in this case, the first point of interest is the trapdoor with medial hinging consisting of the pes anserinus and periosteum. Doing so preserves bone vascularity allowing for improved healing, usually within 6 weeks (Wong and Mahadev 2021). Another point of note was the use of cryoablation as an adjunct to extend the surgical margins, alongside HydroSet® (Stryker Portage, MI, USA) for bone filling. The cryoablation technique, involving repeated cycles of freezing and thawing, would effectively eradicate cancerous cells and also reduces the risk of recurrence (which in the case of chondroblastomas can be as high as 10-35%) (Serrano et al. 2021). Studies have shown that the use of adjuvant cryoablation with surgical curettage do indeed reduce local recurrence and improve patient outcomes compared to surgical curettage alone (Yurtbay et al. 2023). The use of local adjuvants has also enabled less aggressive resections, helping to preserve more bone stock (Apostolopoulos et al. 2024). This is especially important in areas where bone stock is limited such as the subchondral regions. Additionally, cryoablation offers other advantages in terms of its precision and reduced complication rates compared to other techniques such as radiofrequency ablation (Serrano et al. 2021).
With regards to grafting and the choice of cement, HydroSet® (Stryker Portage, MI, USA) was used, a calcium phosphate-based cement to fill in the bone spaces created during curettage to preserve bone integrity and strength. Compared to bone grafting or other synthetic substitutes, HydroSet® (Stryker Portage, MI, USA) offers a quicker turnover time, allowing for effective manipulation and placement within the excised bone space intraoperatively. Alongside proper placement, Hydroset® (Stryker Portage, MI, USA) is also resorbed and replaced slowly which is essential to prevent subchondral bone collapse, by providing structural integrity and preserving the long-term function of the freshly operated knee joint (Schröter et al. 2020).
CONCLUSION
Chondroblastomas are a rare neoplasm affecting children and young adults with nonspecific symptoms and subtle radiograph findings. When examining this particular case, once the patient’s age, history, and epidemiology are considered, and even with relevant imaging done, the misdiagnosis is relatively unsurprising. After all, “common things occur commonly”. It is of no fault that the lesion remained initially misdiagnosed, and this report serves as a learning point for future doctors to consider benign bone tumours as a differential for epiphyseal lesions, especially when there is significant perilesional inflammation as evidenced by increased signal on T2-weighted MRI.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
There are no conflicts of interest.
FINANCIAL SUPPORT AND SPONSORSHIP
None.
INFORMED CONSENT
Consent was obtained from the patient.
AUTHORS CONTRIBUTION
-
Wesford Josh Wei Hock Goh
National University of Singapore, Yong Loo Lin School of Medicine
Email: wesjoshgoh@gmail.com -
Abdul Fattah Lee Abdul Aziz
National University of Singapore, Yong Loo Lin School of Medicine
Email: abdulfattahlee@u.nus.edu -
Arjandas Mahadev
Department of Orthopaedic Surgery, KK Women’s and Children’s Hospital, Singapore
Email: arjandas.mahadev@singhealth.com.sg -
Mohammad Ashik
Department of Orthopaedic Surgery, KK Women’s and Children’s Hospital, Singapore
Email: mohammad.ashik.zainuddin@singhealth.com.sg -
Kenneth Pak Leung Wong
Department of Orthopaedic Surgery, KK Women’s and Children’s Hospital, Singapore
Email: kenneth.wong.p.l@singhealth.com.sg
Wesford Josh Wei Hock Goh (1) and Abdul Fattah Lee Abdul Aziz (2) are co-first authors for this report. Kenneth Pak Leung Wong (5) is the last author.

.png)

.png)


.png)

.png)