Introduction
Sciatic nerve palsy (SNP) after total hip arthroplasty (THA) is a rare and devastating complication, with an incidence of 0.7%-3.7% during primary THA (Patel, Krumme, and Golladay 2021; Brown, Swanson, and Nercessian 2008; Van Der Merwe 2023). Despite a number of known risk factors for SNP after THA, including posttraumatic arthritis, developmental dysplasia of the hip (DDH), and significant limb lengthening, up to 50% of iatrogenic nerve injuries have no known etiology (Hasija et al. 2018; Farrell et al. 2005; Pritchett 2004; Hurd et al. 2006). As the number of joint replacement surgeries performed continues to rise, both surgeons and patients seek techniques which achieve perioperative goals while minimizing complications (S. Kurtz et al. 2007).
SNP is the most common motor nerve injury after THA (Farrell et al. 2005; Schmalzried, Amstutz, and Dorey 1991). Multiple mechanisms have been proposed, including direct compression with errant instrument placement, compression of anatomical structures, excessive traction, and ischemia (Hasija et al. 2018; Farrell et al. 2005; Shetty et al. 2019). Additional mechanisms, such as compression secondary to hematoma (Asopa et al. 2014) and thermal injury due to polymethylmethacrylate, have also been implicated (Birch et al. 1992). A recent study also demonstrated no relationship between surgical approach and risk of SNP [N1]. Despite the extensive role of nerve injury in litigation following arthroplasty (Upadhyay et al. 2007), there remains a paucity of data on the subject (De Fine et al. 2017). In addition, much of the contemporary published data has been the result of single institution studies, which often require the inclusion of patients over several decades due to the rarity of SNP after THA (Farrell et al. 2005; Kyriacou et al. 2013; Park et al. 2013).
With the number of THAs projected to increase each year, a robust understanding of even infrequent complications is crucial as surgeons continue to weigh the risks and benefits of THA. The purpose of this study was to answer the following questions: 1) What is the incidence of SNP after primary THA nationwide; 2) What risk factors associated with developing a SNP after primary THA?
Methods
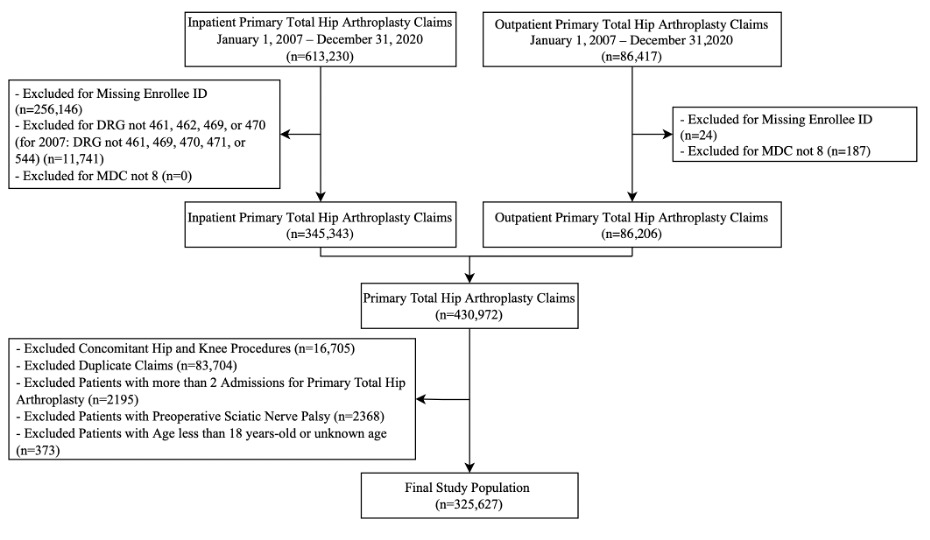
After approval from our institutional review board (IRB), a retrospective cohort study was conducted using MarketScan Commercial Claims Databases. MarketScan is a database of millions of deidentified commercial employer-based health insurance claims in the United States, that allows one to track the healthcare utilization of patients. A total of 325,627 primary THAs in 286,785 patients were identified between January 1, 2007 and December 31, 2020 using the Current Procedural Terminology (CPT), International Classification of Diseases Ninth Revision (ICD-9) Clinical Modification, and International Classification of Diseases Tenth Edition (ICD-10) Procedural Coding System codes listed in Supplementary Table 1. Only cases with a major diagnostic category (MDC) of 8 for Musculoskeletal System and Connective Tissue were included. Cases were excluded if they had concomitant revision THA, hip resurfacing, and/or total knee arthroplasty. Patients were excluded if they had more than 2 primary THAs within the study period. SNPs were diagnosed using the ICD-9 and ICD-10 codes listed in Supplementary Table 1 and must have occurred within 90 days of primary THA. Cases with a history of SNP preoperatively were excluded (See Figure 1).
The database was reviewed for year of surgery, month of surgery, age at time of surgery, gender, and geographical region, as defined by the United States Census Bureau (“Geographic Levels,” n.d.). The Charlson Comorbidity Index (CCI) was calculated using the method outlined by Glasheen et al (Glasheen et al. 2019). Indications for THA and comorbidities present on admission for THA were categorized based on the ICD-9 and ICD-10 codes listed in Supplementary Table 1. Given that 31,523 THAs (9.7%) had multiple indications for THA, the following hierarchy was used to identify the primary indication for THA: DDH, posttraumatic arthritis, osteonecrosis, osteoarthritis, and other indication for THA.
Study Population
Mean age was 56.3 years and 49.3% of patients were women. The south region had the highest proportion of primary THAs (36.7%). CCI was overall low with a mean of 1.6. Comorbidities included: diabetes mellitus (9.4%), benign essential hypertension (40.5%), congestive heart failure (1.3%), peripheral vascular disease (0.7%), lumbar spine pathology (1.1%), anxiety and/or depression (10.9%), history of smoking (7.5%), history of alcohol abuse (1.2%), and history of drug abuse (0.5%) at the time of THA. Primary indications for THA included 81.7% with osteoarthritis, 8.9% with osteonecrosis, 5.4% with other indication for THA, 3.3% of hips with DDH, and 0.8% with posttraumatic arthritis.
Statistical Analyses
Python was used for statistical analysis. Univariate logistic regressions, odds ratios (OR), and 95% confidence intervals (CI) were performed to assess for risk factors for diagnosis of a postoperative SNP. A multivariable logistic regression using year of THA, age, gender, geographical region, CCI, and indication for THA was performed. Alpha was set at p<0.05.
Results
Incidence of SNP
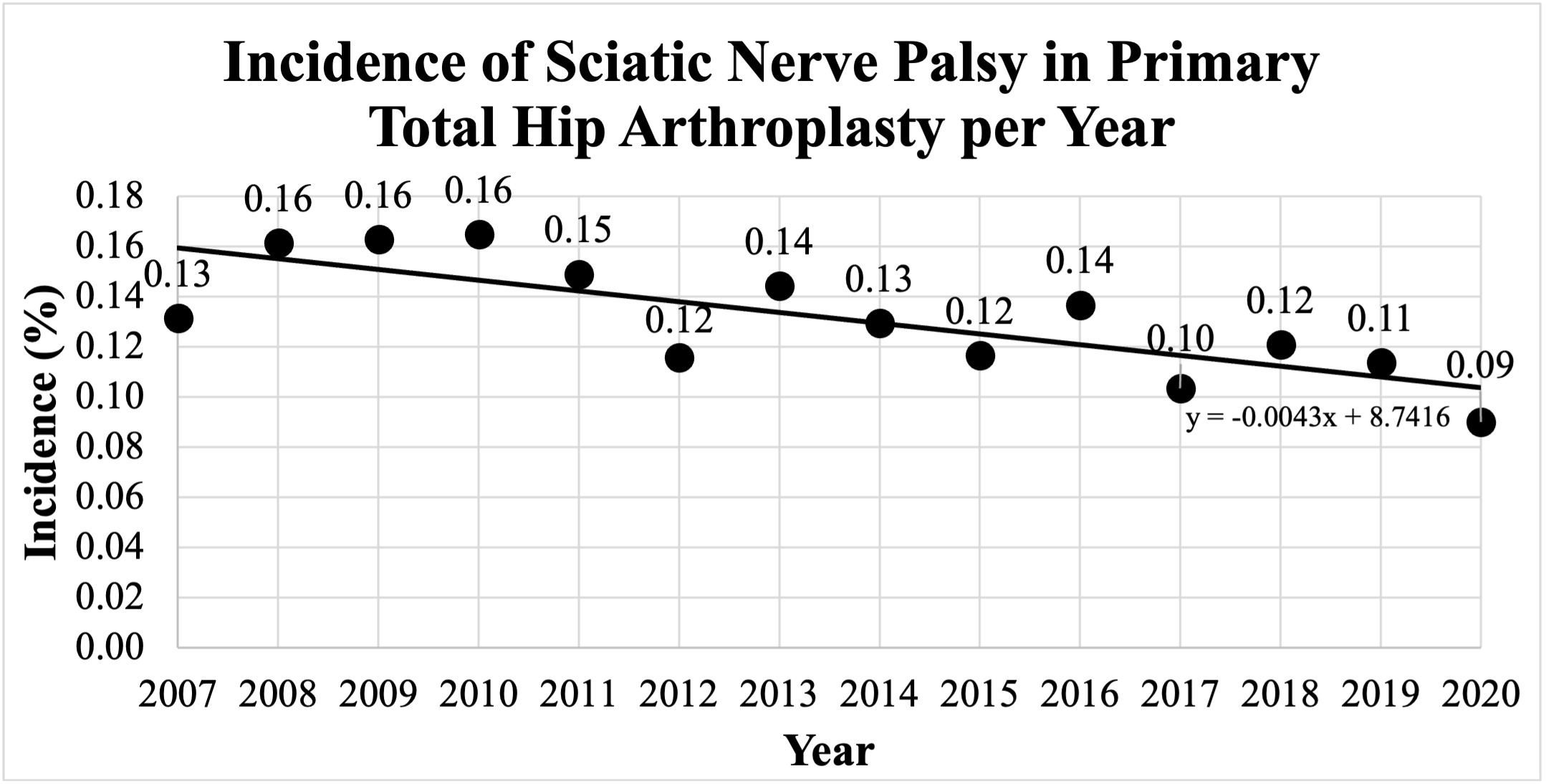
We identified 429 SNPs within 90 days of primary THA for an overall incidence of 0.13%. The incidence of SNP decreased from 2007 to 2020 (p=0.01, See Figure 2).
The incidence of postoperative sciatic nerve palsy after primary total hip arthroplasty decreased from 2007 to 2020 (p=0.01).
Risk Factors for SNP
Patients who sustained a SNP tended to be younger (OR=0.99, p=0.01). Women were 1.7 times more likely to have a postoperative SNP (p<0.001) and people living in the South, which had the lowest incidence of SNP, had a lower risk of being diagnosed with a SNP compared to the Northeast (p<0.001, See Table 1).
CCI was not a risk factor for developing a SNP (p=0.7), but patients who had peripheral vascular disease were 2.5 times more likely to develop a SNP (p=0.02), patients with dementia were 4.2 times more likely to develop a SNP (p=0.04), and patients diagnosed with a malignancy (excluding malignant nonmelanoma of the skin) were 2.0 times more likely to develop a SNP (p=0.04). Other categories of the CCI were not risk factors (See Table 2).
Patients with preoperative lumbar spine pathology were 2.1 times more likely to develop a postoperative SNP (p=0.02). Patients with a documented history of drug abuse were 3.3 times more likely to develop a SNP (p=0.002). Other comorbidities were not found to be risk factors for SNP, including diabetes mellitus (p=0.3), benign essential hypertension (p=0.5), anxiety and/or depression (p=0.1), history of smoking (p=0.5), and history of alcohol abuse (p=0.7, See Table 3).
Undergoing a THA for DDH increased the risk of developing a postoperative SNP 1.9 times compared to osteoarthritis (p=0.004). Similarly, a diagnosis posttraumatic arthritis increased the risk of developing a postoperative SNP 4.0 times compared to having osteoarthritis (p<0.001). Osteonecrosis did not increase the risk of a postoperative SNP compared to osteoarthritis (p=0.8, See Table 3).
A multivariable logistic regression model showed that the earlier year of surgery (OR=0.97, p=0.03), younger age (OR=0.98, p=0.003), women (OR=1.7, p<0.001), higher CCI (OR=1.1, p=0.02), geographical region (p<0.001), and diagnosis of posttraumatic arthritis (OR=4.0, p<0.001) increased the risk of developing a postoperative SNP, while other indications for THA, including DDH (p=0.07), osteonecrosis (p=1.0), and other diagnosis (p=0.06) were not predictive of a postoperative SNP (See Table 4).
Discussion
Infrequent surgical complications remain challenging to study, due to barriers such as small population sizes, institutional bias, and unknown risk factors. The use of nationwide databases may aid in overcoming some of these obstacles.
The current study found the overall incidence of SNP after THA to be 0.13%. This is consistent with previously reported single institution data (Farrell et al. 2005; Park et al. 2013). The significant decrease in incidence during the study period (p=0.01) is interesting and appears to parallel rates of other complications and mortality following THA over time in large scale reviews (Hunt et al. 2013; Partridge et al. 2018). This decrease is likely related to a combination of both surgeon and health care system factors and may be related to increased volume in the use of primary THA nationwide (S. Kurtz et al. 2007). We are hesitant to attribute this to increased use of the anterior approach for THA, since a previously published study demonstrated no difference in the rates of SNP between the direct anterior and posterolateral approaches in THA [N1].
Younger age (p=0.01) and women (p<0.001) were associated with increased rates of SNP after THA. In a recent systematic review, De Fine et al. stated that women and age had been identified as risk factors for SNP after THA infrequently (De Fine et al. 2017). Park et al. demonstrated that patients who sustained common peroneal nerve injuries following THA were significantly younger than those who did not (Park et al. 2013). Comorbidities, such as peripheral vascular disease (p=0.02), dementia (p=0.04), and certain malignancies (p=0.04), were found to be more prevalent in the SNP population. While admittedly outside the scope of this work, the known association between dementia and peripheral vascular disease certainly support ischemia as a possible contributing factor to the development of SNP after THA (Tasci et al. 2018; Owens et al. 2022). However, the risk factors for sustaining a SNP after THA are likely multifactorial.
Previous literature has reported about the relationship between lumbar spine disease and THA. Complications following THA have been found to be increased in patients with both lumbar spine pathology (Blizzard et al. 2017), as well those who have previously undergone lumbar spine fusion (An et al. 2018; Onggo et al. 2020). Similarly, our study found that patients with a history of lumbar spine pathology were 2.1 times more likely to sustain a SNP.
Surgical indication was associated with increased rates of SNP. This study quantified the odds of developing SNP after THA for a diagnosis of DDH to be 1.9 times greater than osteoarthritis (p=0.004). However, posttraumatic arthritis carried a larger odds ratio of 4.0 when compared to osteoarthritis (p<0.001). DDH is a well-studied and known risk factor and often considered directly with postoperative leg lengthening (Schmalzried, Amstutz, and Dorey 1991; De Fine et al. 2017; Pekkarinen et al. 1999). Surgeons should remain vigilant that patients with both DDH and posttraumatic arthritis are at increased risk of SNP.
The generalizability of large database studies remains controversial. In this study, primary THA patients averaged 56 years old and were predominately male. This differs from the 2021 American Joint Replacement Registry (AJRR) data, which found the males made up under 40% of all procedures, with average age of primary THA patients being 66 years old (Siddiqi, Levine, and Springer 2022). As recent studies suggest that the AJRR is representative of nationwide data (Porter et al. 2022), the explanation for this difference is unknown. One explanation may be that insurance payer status skews this population younger and more male, which may help to explain why younger patients continue to rapidly increase their utilization of THA nationwide, which may limit the external validity of this study (S. M. Kurtz et al. 2009).
This study has several limitations. This is a retrospective review using a large database and is subject to errors in coding, omission of coding, and errors in data processing. Additionally, the generalizability of data between demographically different populations remains unknown. The limitations of the data set precluded a more robust analysis of additional demographic factors, use of advanced surgical technologies, and measurement of leg lengthening. Additionally, surgical approach could not be evaluated as it is not part of any medical billing codes. As increasingly large databases with varying benefits and limitations are used to study surgical complications, the authors recognize a possible role for technology such as natural language processing in the future to assist with granular data collection (Wyatt, Booth, and Goldman 2021).
Although its incidence is decreasing, SNP occurs in 0.13% of primary THAs. Younger patients, women, earlier year of surgery, higher CCI, geographical region, and posttraumatic arthritis are associated with increased risk of SNP. In addition, comorbidities that effect nerve vascularity and spinal mobility may be associated with increased risk of the rare yet devastating complication of SNP after THA. Surgeons should continue to seek ways to understand and mitigate risk in their practice.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The views expressed in this article reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
I am a military service member. This work was prepared as part of my official duties. Title 17 U.S.C. 105 provides that "Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. 101 defines a United States Government work as a work prepared by a military service member or employee of the United States Government as part of that person’s official duties.