Introduction
The transforaminal lumbar interbody fusion (TLIF) is a surgical technique that provides decompression of the neural structures as well as circumferential stabilization and fusion of both the anterior and posterior spinal elements. In the traditional open technique of TLIF, the surgery is accomplished through a midline central incision in the patient’s back. Following the skin incision, lumbar spinal musculature is dissected from the spine, and then decompression, placement of spinal instrumentation, and fusion is performed. The open muscle dissection results in significant blood loss. As a consequence, a significant percentage of patients who undergo an open TLIF procedure require some type of blood transfusion following surgery. In the United States, open spinal fusion surgery is one of the top ten reasons that patients receive a blood transfusion, with up to 17% of cases requiring a transfusion in recent years (Aoude, Nooh, Fortin, et al. 2016).
The last two decades have given rise to minimally invasive surgical (MIS) techniques for lumbar spinal decompression and fusion. The mini-open MIS-TLIF surgery is performed through two small paramedian incisions as opposed to a single midline incision. Following the skin incision, an expandable retractor system is deployed to provide a narrow aperture to the spine. Through this narrow window, the surgeon can perform surgical decompression of the nerves, restore disc height with an interbody spacer, and implant pedicle screws for immediate stabilization. In addition, both a posterior lumbar interbody fusion and posterolateral fusion can be achieved through the same exposure.
In contrast to open surgery, the MIS technique does not require dissection of the midline band of paraspinal muscles, thus allowing the band to remain attached to the posterior spinal elements. This decreased degree of muscle dissection results in a much lower rate of blood loss than the traditional open TLIF surgery.
The purpose of this study is to examine the incidence of blood transfusions following MIS-TLIF surgery utilizing the dual incision MIS technique as compared to the traditional open TLIF procedure.
Methods
We retrospectively reviewed a series of 620 consecutive patients who underwent single and multilevel mini-open TLIF surgeries. No patients who underwent the procedure were excluded from the series. The patients’ ages ranged from 20 to 88 years with a median of 54 years. The patient population included 288 males and 332 females (Table 1).
Moreover, we conducted a retrospective review of a series of 33 patients who underwent open TLIF surgeries by the same surgeon from 2005-2013, which provided a foundation of observational data with which to compare operative outcomes. The age of patients in the Open TLIF series ranged from 34 to 84 years with a median of 60 years. The patient population included 10 males and 23 females (Table 1).
Indications for surgeries included but were not limited to: degenerative spondylolisthesis, recurrent disc herniation, isthmic spondylolysis, iatrogenic instability secondary to removal greater than 50% of the facets bilaterally, degenerative disc disease, and traumatic spondylolisthesis. The majority of the 620 patients included in the study presented with two or more indications upon initial consultation (Table 2).
Surgeries were performed in a consecutive manner over 16 years. Every patient had a hemoglobin and hematocrit level test on the first post operative day. After that test, they were followed for at least 90 days for clinical signs of significant anemia. The threshold to transfuse was based on a hemoglobin less than or equal to 7 g/dl in healthy individuals and 8 g/dl in individuals with coronary artery disease. Operative reports, hospital records, and at least three months of clinical follow-up were reviewed for evidence of a need for blood transfusion in the operative or post-operative period. An additional literature review was conducted to identify the incidence of blood transfusion in patients undergoing open Posterior Lumbar Fusion Surgery in other case series.
Surgical Technique
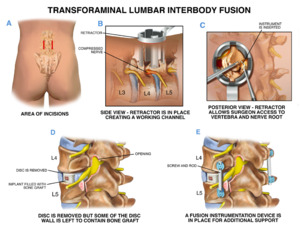
All 620 patients included in the study were treated with a mini-open TLIF technique. The procedure is performed with the patient placed prone on a Jackson table. All pressure points are padded while the patient is under general anesthesia. AP fluoroscopy is used to identify the mid-sagittal plane as well as pedicle screw entry sites of the impacted levels. Two separate paramedian incisions are made 3.5 cm lateral to the mid-sagittal plane that extend from pedicle screw entry site to pedicle screw site (Figure 1A). After the first incision is made in the skin and the lumbar dorsal fascia, blunt dissection is performed with the placement of sequential dilators and an expandable retractor under fluoroscopic visualization to expose the pedicle screw entry site (Figure 1B). Pedicle screws are then placed on the side contralateral to decompression under fluoroscopic visualization. Each pedicle is tapped under continuous electrophysiological stimulation and EMG monitoring. Further electrophysiologic stimulation of the screws is used to confirm appropriate placement of the instrumentation. Finally, appropriate screw placement is further confirmed by AP and lateral fluoroscopy.
A secondary incision is made 3.5 cm from the contralateral mid-sagittal plane and the lumbar dorsal fascia is divided. A secondary retractor is then placed on the contralateral lamina and facet under fluoroscopic visualization utilizing blunt dissection. With the use of the operative microscope and drill, surgical decompression is performed (Figure 1C). The nerve root is gently retracted to allow for discectomy. Then, sequential dilators are used to gradually restore disc height. The contralateral pedicle screws are tightened to maintain distraction and curets are employed to aggressively remove cartilage and disc from the endplate until there is healthy bleeding bone above and below the operative site.
Posterior Lumbar Interbody Fusion is performed by placing a mixture of bone fusion extender and harvested autologous bone from the facetectomy at the end of the disc space. An interbody device is then packed with bone graft extender and autologous bone from the facetectomy and placed into the disc space to fuse the anterior column and provide immediate support (Figure 1D). The retractor is then repositioned, allowing pedicle screws placed on the decompressed side to be interlinked with cross connector set screws (Figure 1E).
Assessment of Results
The operative reports and hospital records of each patient in both the MIS-TLIF and Open-TLIF series were analyzed for evidence of intraoperative or post-operative blood transfusion. Review of the incidence of blood transfusion following Open Lumbar Spine Fusion surgery in the authors’ series of 33 patients revealed an incidence of 15%, while additional literature review of the same procedure revealed a comparable incidence of approximately 17% in recent years (Aoude, Nooh, Fortin, et al. 2016).
Results
620 consecutive MIS-TLIF surgeries were performed by one surgeon over a span of sixteen years. Medical records revealed a numerical estimated blood loss in 511 cases out of 620 (Table 3). The range of estimated blood loss for these 511 cases was 10 cc to 750 cc, with a median blood loss of 100 cc and mean blood loss of 136 cc. In the remaining 109 cases, blood loss was deemed minimal, and a specific numerical value was not assigned. Hospital records for all 620 cases revealed that zero patients required a blood transfusion during surgery or during hospitalization following surgery. This includes cell saver, autologous blood, or any banked blood. Furthermore, at thirty-day post-operative follow-up, zero patients out of 620 required transfusion.
In contrast, medical record review of the authors’ 33 Open TLIF procedures within the same time period revealed a numerical estimated blood loss in 27 out of 33 cases (Table 3). The range of estimated blood loss for these 27 cases was 150 cc to 1000 cc, with a median blood loss of 300 cc and mean blood loss of 370 cc. The remaining 6 cases had minimal blood loss, and a specific numerical value was not assigned. 15% of these patients received some form of blood transfusion, equivalent to 93 cases out of 620. The difference of 93 expected transfusions in 620 open-TLIF surgeries to 0 observed transfusions in 620 MIS-TLIF surgeries is statistically significant using Fisher’s Exact Test (p<0.05).
Discussion
Lumbar spine fusion is one of the most common surgical procedures performed in the operative management of adult degenerative spine disorders. The goals of these surgeries include decompression of the neural elements and stabilization of the vertebrae. Open-TLIF is one such lumbar spinal fusion surgery (Harms and Rolinger 1982; Rosenberg and Mummaneni 2001; Tormenti, Maserati, Bonfield, et al. 2012). This technique affords the surgeon the ability to decompress the neural elements, restore disc height with an interbody space, achieve interbody and posterolateral arthrodesis, and place pedicle screw instrumentation. All of this is done through a single midline incision with subsequent muscle dissection of the paraspinal muscles from the lamina and facets.
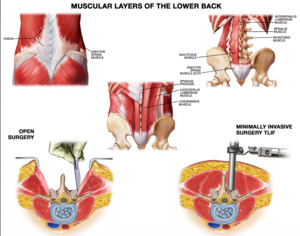
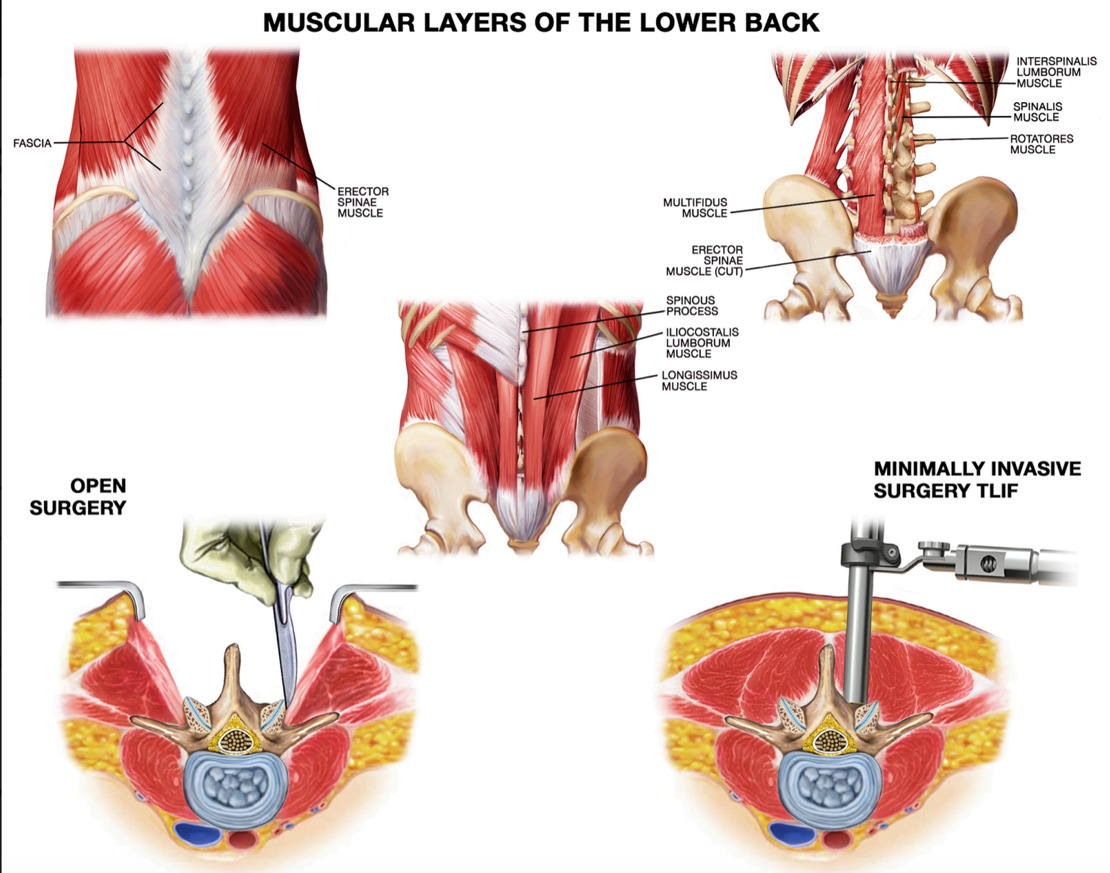
One significant disadvantage of the Open-TLIF technique is the large degree of muscle dissection required to achieve desired decompression (Aoude, Nooh, Fortin, et al. 2016). The surgical exposure in the Open-TLIF surgery requires the dissection and detachment of four key structures of the lumbar spinal region. First, the lumbodorsal fascia must be completely disconnected from the spinous processes of the target level as well as the levels above and below. Second, the Multifidus muscle must be detached and dissected from the mamillary processes of the lumbar spine over several segments. Third, the Spinalis component of the Erector Spinae muscle must be detached from multiple levels of spinous processes. Fourth, the Longissimus component of the Erector Spinae must be detached from the transverse process origins and insertions over multiple segments beyond the target level. This detachment of the paraspinal muscles from the posterior spinal elements during open surgical exposure often results in significant blood loss (Figure 2).
Consequently, many patients who undergo open posterior lumbar fusion surgery require post-operative blood transfusions. In fact, open spinal fusion surgery is one of the top ten surgeries associated with blood transfusions in the United States (Segal, Guallar, and Powe 2001). Basques et al. observed a 16.7 percent transfusion rate amongst 4223 patients who underwent open posterior lumbar interbody fusion procedures (Basques, Anandasivam, et al. 2015). In a study published three years later, Morcos et al. observed a transfusion rate of 18 percent amongst 722 patients who underwent open posterior spinal fusion (Morcos, Jiang, et al. 2018).
The last 25 years have afforded substantial advancement in spinal fusion surgery with the rise of minimally invasive surgery (MIS). MIS techniques incorporate a fixed or expandable tubular retractor system that achieves surgical exposure of the spine without stripping the paraspinous muscles directly from the spine. The use of the expandable retractor system in lumbar MIS surgery provides four key advantages over open lumbar spine surgery. First, it allows for preservation of the interspinous ligament and its associated lumbodorsal fascia, which is a key origin and insertion point for all three muscle layers of the back. Second, the expandable retractor helps avoid complete dissection of the spinalis muscle from the spinous processes. Third, the expandable retractor allows for preservation of the Longissimus and Multifidus muscles. Finally, the MIS technique allows the surgeon to minimize the area of muscle dissection to just the target levels of the spine, rather than having to extend the muscle dissection beyond the scope of treatment as is traditionally required in the open procedure.
Dr. Richard Fessler was an early pioneer in the development of the MIS-TLIF procedure (P. Lee and Fessler 2012; Wong, Smith, Nixon, et al. 2015). His technique included surgical decompression of the neural elements through a tubular retractor followed by percutaneous placement of pedicle screws. Further modification of this minimally invasive technique by Drs. Sanjay Dhall, Michael Wang, and Praveen Mummaneni resulted in the mini-open TLIF technique, which utilizes two separate incisions approximately 3 to 4 cm from the midline to access both sides of the spine (Dhall, Wang, and Mummaneni 2008). An expandable tubular retractor is used to maintain a pathway to the spine. This dual incision mini-open TLIF approach provides the surgeon with a direct visual corridor to the lamina, facet, and transverse process, all while preserving the attachment of the Longissimus paraspinal musculature.
While literature published by these pioneers and others support the observation of a significant reduction in blood loss with the MIS technique compared to the Open procedure, the utility and complication rates of MIS-TLIF procedures has been analyzed in variable patient sample sizes (Table 4). Dr. Mummaneni’s team series observed a mean estimated blood loss (EBL) of 194 cc in 21 MIS-TLIF patients, compared to 505 cc in 21 Open TLIF patients. Dr. Fessler’s team presented the intraoperative and perioperative complications of 513 MIS-TLIF surgeries. In his team’s series, 2 of the 513 patients required post-operative blood transfusion following surgery, equivalent to a 0.4 percent incidence of blood transfusion (Wong, Smith, Nixon, et al. 2015).
Villavencio et al. observed a statistically significant reduction in blood loss when comparing minimally invasive to open TLIF surgeries in a series of 139 patients (Villavicencio et al. 2010). 76 patients underwent spinal fusion surgery with the MIS technique and 63 patients underwent spinal fusion surgery with the Open technique. The mean estimated blood loss for MIS-TLIF patients was 162 cc compared to 366 cc for their Open-TLIF patients. Of their 76 patients that underwent a MIS-TLIF procedure, one required a post-operative blood transfusion, equivalent to a blood transfusion incidence rate of 1.3 percent in their series.
Our study is unique in that it represents the efforts of a single surgeon over a period of 16 years with 620 consecutive MIS-TLIF surgeries, the largest study population of its kind. No patients who underwent the procedure were excluded from the series. In this contiguous series, no patients required a post-operative blood transfusion. Our zero percent incidence is lower than in currently available MIS-TLIF literature and is in stark contrast to the 16 to 20 percent incidence of transfusion witnessed in Open-TLIF surgeries.
We identify two likely reasons for the reduction in transfusion incidence: incision size and the degree of required muscle dissection. First, in MIS surgery, the size of the surgical incision is smaller and more targeted than that of Open-TLIF surgery. In the case of an L4-5 fusion with the MIS technique, each incision extends from the transverse process of L4 to the transverse process of L5. On the other hand, L4-5 exposure utilizing an Open-TLIF method requires a midline incision that typically extends from the top of the L3 spinous process to the midsacrum. This larger incision results in greater tissue dissection and potential blood loss.
Second, the degree of muscle dissection in the MIS-TLIF technique is significantly less than what is required with the open technique. In the open TLIF surgery, the Longissimus, Spinalis, and Multifidus musculature are all dissected from the spinous process, lamina, and transverse processes of the spine (Figure 2). Furthermore, the key lumbodorsal muscle groups are completely detached from their primary point of insertion, the Supraspinal Ligament. In contrast, the dual incision MIS technique requires a blunt channel through the left and right erector spinae groups, with each incision 3.5 centimeters from midline (Hoh, Wang, and Ritland 2010). As a consequence, the central 7 centimeters of the left and right erector spinae musculature of the longissimus and spinalis groups are left undissected in the MIS exposure (Figure 2). Furthermore, the key attachment of the posterior lumbar musculature into the spinous process and Supraspinous Ligament are unaffected in the MIS-TLIF technique. This reduction in the degree of muscle dissection is the most likely reason for the dramatic difference in the incidence of blood transfusion between open and MIS-TLIF techniques.
The benefit of reduced blood loss is particularly important in obese patients (BMI, >30), who often have a much deeper surgical field in open lumbar spinal surgeries as compared to patients with a normal BMI (18.5-24.9). As a result, a larger incision must be made to expose deep surgical fields in obese patients compared to fields in patients with a normal BMI. This is a likely reason that obese patients who undergo open lumbar spine surgery typically experience greater blood loss compared to their peers with a normal BMI (Rosen et al. 2008).
In contrast, the size of the incision in MIS-TLIF procedures is not affected by the depth of the surgical field. The expandable retractor system affords a sustained corridor to the spinal anatomy regardless of depth of field; therefore, the same sized incision can be used on an obese patient as a thin patient in MIS-TLIF surgery. Consequently, Rosen et al. observed no statistically significant difference in the blood loss of obese patients who underwent MIS-TLIF surgery compared to patients with a normal BMI who underwent MIS-TLIF surgery (Rosen et al. 2008).
The primary limitations of this study are that it is a retrospective study without any randomization of the patients between open and minimally invasive surgery. As the primary surgeon gained experience and comfort with the minimally invasive approach, the open technique was gradually phased out of the practice, as represented by the significant difference in the number of patients who underwent lumbar spinal fusion with the minimally invasive approach as compared to the open approach. Due to the marked decrease in morbidity with the minimally invasive approach compared to the open, it is unlikely that any surgeon would agree to a randomized trial to further the validity of the MIS technique.
In summary, the MIS-TLIF surgical technique results in significantly less blood loss compared to the open technique. Current literature supports this fact; however, this study adds a significant volume of data-driven evidence to support this conclusion. This is the largest single-surgeon case series to show consistent absence of blood transfusions over sixteen years and 620 consecutive cases of MIS-TLIF surgery. Further study is required to determine whether there are additional benefits of MIS techniques in spinal surgery, particularly as it relates to the duration and extent of functional recovery following surgery.