Introduction
Presented is a case of bacterial osteomyelitis of the proximal ulna initially diagnosed as olecranon bursitis. The patient was successfully treated with irrigation and debridement followed by PO antibiotics. This case illustrates the subtle distinction between low-grade osteomyelitis and soft tissue inflammation such as bursitis. To the authors’ knowledge, this is the first reported case of olecranon osteomyelitis caused by Aeromonas sobria.
Case Report
A 71-year-old immunocompetent female with a past medical history of osteoporosis, hyperlipidemia, and hypothyroidism presented to her primary care physician with a 1-month history of swelling over the posterior left proximal forearm. Initially painless, she reported that shortly after lightly bumping the elbow, she experienced significant pain, decreased range of motion, and warmth of the affected area. Of note, during this traumatic bump, there was no exposure to brackish water or water exposure of any type. No bruise, cut, or lasting scrape was associated with the elbow trauma. Associated symptoms were relieved with ibuprofen and lasted approximately 24 hours before resolving, after which she developed localized edema. She denied fever, chills or other constitutional symptoms. She related a remote history of left ipsilateral radial head fracture that had been managed nonoperatively and denied any recent febrile illness or traumatic or penetrating injury prior to the onset of symptoms. Upon physical exam, the patient was noted to have a non-tender fluid collection measuring approximately 5cm x 5cm over the proximal ulna. There were no overlying skin changes and no drainage. She was diagnosed with possible olecranon bursitis and was referred to an orthopedic upper extremity surgeon’s office for further evaluation.
A physical exam performed by the orthopedist was noted to show soft tissue swelling at the proximal ulna, about 2 cm distal to the olecranon tip. There was minimal erythema and no tenderness to palpation. Due to the location of soft tissue swelling just distally to the olecranon tip, the orthopedic surgeon wanted to rule out involvement of the ulnar bone in this case. X-rays obtained and interpreted by the orthopedist demonstrated a moth-eaten appearance of the proximal ulna (Figure 1). With radiographic findings concerning for osteomyelitis versus neoplasm, an MRI was ordered.
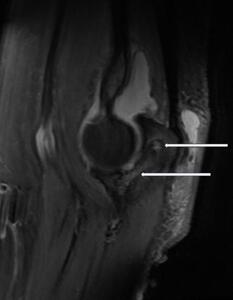
The MRI, performed 5 days later, demonstrated bone marrow high signal, confirming the suspicion of chronic olecranon osteomyelitis, with decompression into the olecranon bursa via a dorsal cloaca (Figure 2). With no evidence of hypointense tumor marrow involvement, bony neoplasm was considered less likely than osteomyelitis following MRI. The MRI also suggested decompression into the joint through the olecranon articular surface, and identified moderate joint effusion and olecranon bursitis with a 0.8 cm ossific body.
Subsequently, the patient was taken to the operating room for exploration with irrigation and debridement of the involved bone. Intraoperative findings included a lytic area in the proximal ulna with loss of trabecular architecture. Intraosseous cultures were collected. The olecranon bursa was completely excised and then sent for pathologic examination.
On postoperative day three, Aeromonas sobria was detected in the tissue culture. The patient was referred to an infectious disease specialist, who recommended levofloxacin 750 mg PO for 42 days. Approximately one month after surgery, the patient returned to the orthopedic surgeon for evaluation. Significant improvement on the physical exam was noted. X-rays revealed what appeared to be osseous integration at the previous lytic area (Figure 3). PO antibiotics were continued.
At the two-month follow-up, the patient was found to have full motion with a normal exam and continued improvement on the x-ray after PO antibiotics. She was discharged with instructions to return as needed. She has achieved a full range of motion and there is currently no radiographic evidence of ulnohumeral arthritis resulting from the possible intra-articular penetration seen on MRI. At long-term follow up, the patient has a normal exam with no pain or limitations to range of motion.
Discussion
Osteomyelitis is an inflammatory process involving the bone, which occurs secondary to infection. Osteomyelitis can be hematogenous, which is secondary to blood infection, and nonhematogenous, which occurs from direct inoculation in a trauma or surgery setting or is spread through soft tissue/joint infections. Symptoms may include erythema, swelling, calor, pain, fever, or chills (Momodu and Savaliya 2020). In this case, due to the lack of open wound, this case of osteomyelitis was likely due to hematogenous spread. Olecranon bursitis is an inflammatory process of the bursa, which may be caused by trauma, prolonged pressure, autoinflammatory conditions, or infection. The appearance of olecranon bursitis is characteristically a round, golf-ball-shaped protrusion at the tip of the elbow, due to the fluid’s enclosure within the bursa. Bursitis may be infected (septic) or sterile. The presentation of bursitis may closely resemble osteomyelitis, with common symptoms including erythema, tenderness, malaise, and in a majority of septic olecranon bursitis cases, fever (Pangia and Rizvi 2020).
To the authors’ knowledge, this is the first recorded case of Aeromonas sobria leading to osteomyelitis. Based upon a 1988 study of Aeromonas infections in California over 12 months, the incidence of Aeromonas infection in the general population is very low, approximately 10.6 in one million patients (King, Werner, and Kizer 1992). Moreover, of all Aeromonas infections, sobria accounts for only about 30 - 40 % of infections (Pessoa et al. 2022).
In 2023, a Norwegian study estimated the rate of wound infection by Aeromonas at .2 per 100,000 inhabitants, further illustrating the rarity of this case (Hyllestad and Amato 2023). Unfortunately, literature review globally and locally on Aeromonas infections is limited by the fact that Aeromonas infections are no longer reportable in most countries, including the United States. In immunocompetent individuals, this literature review also becomes limited, as Aeromonas bacteremia most often occurs in the cases of malignancy and cirrhosis (Katz et al. 2015). It is clear, however, that osteomyelitis of the proximal ulna is also in itself rare. In a retrospective study of 344 bacterial osteomyelitis patients in Spain, only 4 patients presented with osteomyelitis in the ulna (García Del Pozo et al. 2018). Other population-based studies in India and China respectively have reported the incidence of osteomyelitis of the ulna to be between 0.8% and 1.86% (Khonglah et al. 2020; Jiang, Ma, Jiang, et al. 2015). In context, this case serves as a unique intersection of the infrequent occurrence of ulnar osteomyelitis and the rarity of Aeromonas infections.
The presentation of osteomyelitis infection by Aeromonas sobria in this case was qualitatively different from reported cases of osteomyelitis caused by other species of the Aeromonas genus. In a case of osteomyelitis caused by Aeromonas hydrophila, a delayed complication of an open reduction and internal fixation of the right lower limb was reported. This led to symptoms of pain, fever, or purulent drainage from the site of surgery at 6 months, after which it was treated with levofloxacin 750 mg BID. Notably, in our reported case, there was no fever or purulent discharge, which could point to differences in the manifestation of symptoms between A. hydrophila and A. sobria. In both cases, the infection responded to treatment, and the Aeromonas bacteria was the only pathogen identified in a bacterial culture (Agrawal et al. 2017).
This case of osteomyelitis caused by Aeromonas sobria is notable both for its presentation and the organism involved. As mentioned, Aeromonas has rarely been reported, and A. sobria of the proximal ulna appears to be unique in the medical literature. Additionally, the benign presentation, without fever, pain, erythema, and with swelling near the olecranon, could easily have been misdiagnosed as olecranon bursitis.
X-rays are not routinely ordered when bursitis is the working diagnosis, and in this case, the initial radiographic findings were subtle. Consequently, MRI was very helpful in making the decision for operative irrigation and debridement. In the future, MRIs may be used to better differentiate between osteomyelitis of the ulna and olecranon bursitis in situations where the distinction is not clear.
Illustrated in this case report is the importance of a detailed history and physical exam. While the initial impression was that of straightforward olecranon bursitis, certain features of the clinical presentation were atypical, such as brief severe pain that resolved prior to the onset of the swelling; in addition, the location of the swelling was distal to the olecranon tip. A more typical presentation would include swelling over the tip of the olecranon with contemporaneous pressure-like discomfort. These subtle differences created uncertainty regarding the diagnosis and prompted orthopedic surgery referral which led to the timely diagnosis and treatment of osteomyelitis.
Abbreviations
PO: Per orem, or by mouth
BID: Twice per day
MRI: magnetic resonance imaging