Introduction
Within medicine, surgical specialties are unique in that trainees must face a sharp learning curve regarding learning operative skills. Historically, the only way to improve surgical technique outside the operating room was by using cadavers and models (Crockatt et al. 2023). Recently, there has been more emphasis placed on extended reality (XR) systems to provide residents with high-quality training in various scenarios outside of the operating room. XR systems including visual interface modalities such as virtual reality (VR), augmented reality (AR), and mixed reality (MR) provide immersive experiences by combining virtual environments with the real world (Curran et al. 2022). As these systems have continued to progress, so have their utility in bridging the steep learning curve of operative medicine. Currently, these devices are capable of simulating procedures in multiple surgical specialties (Gupta et al. 2024; Hakky et al. 2016; Bui et al. 2024; Portelli et al. 2020). The efficacy of these systems is supported by an increasing body of literature suggesting that utilization of XR technologies may improve surgical outcomes by reducing both navigational speeds and error (Bollen et al. 2022; Guha et al. 2023). Further, there have been reports of XR training allowing for greater consistency and improved skill progression (Guha et al. 2023; Keith, Hansen, and Johannessen 2018).
Within the field of orthopedic surgery, the potential of XR as an adjunct to the surgeon intraoperatively is just recently being explored, such as in hip, shoulder, and knee arthroplasty (Hasegawa et al. 2023; Sanchez-Sotelo et al. 2024; Tsukada et al. 2023). Alongside these studies, there are emerging reports of implementation of XR technologies as a tool for orthopedic surgery trainees outside of the operating room, with promising results (Hasan et al. 2021). Although these technologies have become more common, the views of trainees on these purported benefits of XR remain underreported (Kuhn et al. 2024). Our study seeks to understand the perceptions of orthopedic surgery trainees regarding the utility, accuracy, and barriers to widespread integration of XR systems into orthopedic training programs.
Methods
Survey Design and Administration
This study was designed as a cross-sectional survey which was administered using Qualtrics to assess orthopedic residents’ perceptions on the use of mixed reality in orthopedic surgery training. The survey was composed of 18 questions (Supplementary Table 1) which were divided into five sections: demographics, perceived need for XR in orthopedic training, accuracy of XR for simulating orthopedic procedures, ability of XR to enhance skill training, ability of XR to improve clinical outcomes, and challenges/barriers to integration of XR into orthopedic surgery training. The survey contained an initial mandatory question to validate the responder was an orthopedic surgery resident. If the respondent did not answer the question or was not a trainee, the survey was automatically ended. For survey questions which evaluated respondent agreement a modified Likert scale was used. As such, users rated their level of agreement with the following scores: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree.
Prior to administration, the survey was validated internally for accuracy by two orthopedic surgery residents (MT and TW). The survey was then sent to all orthopedic surgery program coordinators within the US with the intended distribution of the survey to all orthopedic residents within the respective program. The survey was also distributed via social media. Survey data was only accessible by one author (NG) to maintain privacy.
Data Reporting
First, in order to ensure no duplicate responses were included in the analysis, responses were determined to be unique using the IP address, time, and location of the responder. Responses were then considered complete if ≥ 70% of questions were completed. For reporting of demographic results, all responses were included. For reporting of perceptions on XR use, only responses with ≥ 70% completion were included. Additionally, responses were stratified by those with and without XR use. Finally, for reporting of respondent perceptions within our results section, overall disagreement includes Likert score 1 and 2, while overall agreement is indicated by Likert scores of 4 and 5.
Results
Demographic Results
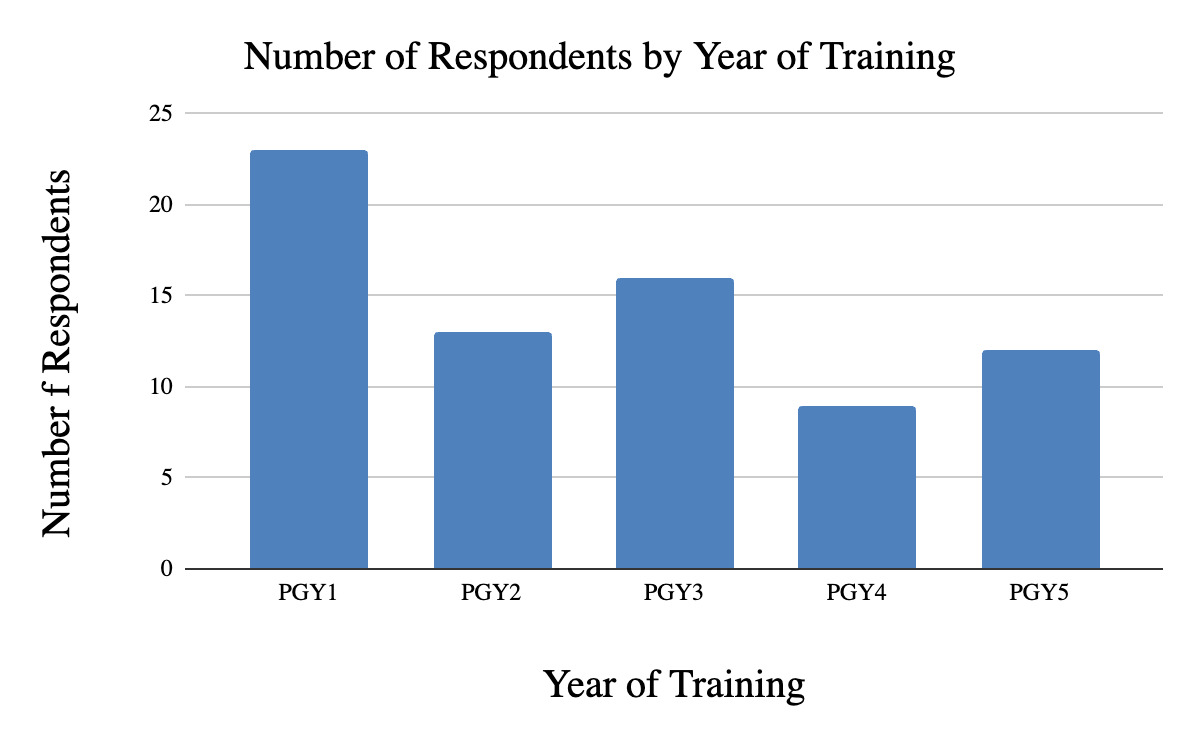
The survey received a total of 78 responses, of which 55 (70.5%) were ≥ 70% completed. Survey responses were indicative of perceptions from all levels of orthopedic surgery residency, with the majority in their first year of residency (Figure 1). There were 21 unique institutions represented and the majority of respondents (69.1%) indicated that their training institution did not use XR. Of those that did use XR, reported technology varied and included arthroscopic simulators and VR headsets. The most common subspecialty for which XR was used were hip/knee (28.2%), followed by sports medicine (25.6%) and shoulder/elbow (17.9%) (Table 1).
Survey Results
Survey results overall and stratified by access to XR are visualized in Figure 2-4. Most respondents agreed that there is a need for surgical skill training outside of the operating room (87.18%), however, overall agreement was more neutral regarding the need for XR specifically to improve the training of orthopedic surgeons (33.35% agreed) and if all orthopedic surgery training programs should offer access to XR simulators (17.84% agreed).
In regard to the technical accuracy of XR, 25.46% of participants agreed or strongly agreed that XR provides an accurate simulation of orthopedic procedures while 36.36% were neutral. These results were similar for statements regarding XR’s ability to accurately model patient-specific anatomy for pre-operative planning (36.36% agreed or strongly agreed) and its ability to create an accurate simulation of the operating room environment. For improving procedural confidence, 67.28% of participants agreed/strongly agreed that XR can improve resident procedural confidence. Positive perceptions were additionally reported for if the use of XR during training can improve skill progression (65.46% of participants agreed or strongly agreed).
The perceived impact of XR use during training and its subsequent impact on patient outcomes was also assessed. There was overall disagreement regarding XR’s ability to reduce inpatient length of stay with 40% of respondents indicating neutrality and only 7.27% agreed or strongly agreed. Similarly neutral responses were conveyed regarding the ability of XR to improve the accuracy of hardware/prosthetic placement (30.91% neutral). A total of 45.45% of respondents agreed with the ability of XR to reduce navigational error, while 10.91% disagreed. Finally, most respondents felt neutral (50.91%) or disagreed (27.27%) that mixed reality can relieve surgeon discomfort and/or improve fatigue.
Finally, the perceived barriers to integration to XR were evaluated. Respondents were predominantly neutral (54.55%) on their perception of mixed reality systems being easy to use. Notably, participants with access to mixed reality systems were more likely to agree that XR systems are easier to use than participants whose programs did not have access to XR systems. This suggests that familiarity with XR systems may influence participant comfort. Most participants (52.72%) agreed that the largest barrier to integration of XR is cost followed by a lack of dedicated time to use the technology during their training program (34.55% agreed or strongly agreed). In contrast, only 27.27% of participants agreed that insufficient education on how to use XR system technology was the largest barrier.
Discussion
We surveyed orthopedic surgery trainees nationwide to better assess their opinions regarding the growing use of XR within orthopedic training education. Responses were received from trainees from 21 institutions across the United States. Of the gathered responses, 69% indicated that they currently do not have access to XR systems, while 31% do have access to these training systems. Various forms of XR are currently used in orthopedics, as indicated by our results, with its application particularly limited to education and preoperative planning (Verhey et al. 2020). Current systems available by orthopedic trainees are most seen in trauma, joints, spine, and oncologic procedures (Bian et al. 2024). Interestingly, our results indicated the most common uses were in joint procedures. However, data regarding trauma, spine, and orthopedic oncology simulation was limited. Although these technologies are becoming more common as there is promising evidence for their efficacy as a training adjunct, they are still in their infancy and not yet a mainstay across many orthopedic surgery programs.
In its current state, XR has the potential to help orthopedic trainees with their understanding of fractures, creation of treatment plans, and accuracy with screw and other instrument placements during surgery (Hasan et al. 2021; Javaid et al. 2019). The efficacy of XR in improving surgical skills has been shown in the literature using trainees of all levels. In medical students, Orland et al. demonstrated that first and second-year medical students without prior experience in tibial intramedullary nail procedures had greater step completion rate, decreased incorrect steps, and shorter completion time after VR training (Orland et al. 2020). Similar results were then shown in a larger cohort of VR-trained senior medical students who had faster tibial intramedullary nail procedure completion times than those given a standard industry surgical technique guide (Lamb et al. 2023).
Multiple studies have evaluated the benefit of VR in orthopedic junior residents, with most of the literature focusing on arthroplasty techniques. Examples of this include a randomized controlled trial of 14 orthopedic surgery interns performing cadaveric total hip arthroplasty (THA). The half receiving additional VR training outperformed those with only cadaveric training in scoring of cadaveric THA and technical performance (Hooper et al. 2019). Similarly, Logishetty et al. demonstrated that in 24 surgical trainees with no prior experience of anterior approach THA, VR-trained orthopedic surgical trainees completed more key steps, were more accurate in component orientation, and had faster operative times in performing a cadaveric THA compared to those who had used conventional preparatory materials (Logishetty, Rudran, and Cobb 2019). Importantly, Mckinney et al. demonstrated the use of XR in newer procedures which are becoming more integrated into orthopedic surgeons training. In their study of 22 orthopedic surgery residents performing a unicompartmental knee arthroplasty with an immersive VR system, there was greater successful completion of procedural steps and faster operative times. These promising results are also supported in senior residents with significant reductions in errors, speed, completion of procedural/critical steps, and instrument handling in procedures such as shoulder arthroplasty (Lohre, Bois, Pollock, et al. 2020; Lohre, Bois, Athwal, et al. 2020).
As it is clear from the literature XR technologies are effective adjuncts for trainees at all levels, it is important to note that 65% of respondents agreed that XR use could improve skill progression. This is a crucial finding of our study as it aligns with the literature suggesting these technologies may reduce the learning curve for junior residents, providing foundational practice for improved technical skills early on (Orland et al. 2020; Lamb et al. 2023). Interestingly, residents with access to XR expressed a higher degree of confidence in the direct translation of skills learned in the operating room than those who did not have access to the technology, which is consistent with the current literature (Lohre, Bois, Pollock, et al. 2020; Lohre, Bois, Athwal, et al. 2020). There was also increased confidence in XR’s ability to simulate the operating room accurately in trainees with XR access compared to those without. The decreased confidence among trainees without XR could potentially be attributed to preconceived ideas of the current technology available. A similar trend was seen in questions regarding reduced navigational error and improved accuracy of screw/prosthetic placement, with less agreement in those without access to XR. With current evidence to support the usefulness of XR for not only procedural confidence but also improved technical skills and surgical accuracy, it may be important for training programs to understand the utility of XR through implementation of pilot programs.
With the rapid growth of XR, a major point of contention is the ability of these devices to reduce the physical strain and fatigue of surgeons intraoperatively. Although musculoskeletal injury secondary to ergonomics in the operating room are a leading cause of occupational injury in orthopedic surgeons (Tan and Kwek 2020), there was relative disagreement among respondents (even when stratified by access) regarding XR’s ability to reduce surgeon discomfort/fatigue. As most of the literature supporting decreased fatigue is focused on spinal surgery, further understanding of the potential effect of XR in other orthopedic subspecialties is warranted (Sakai et al. 2020). Of note, the potential for unnecessary visual fatigue is another frequently discussed drawback. This phenomenon is known as cybersickness: the combination of uncomfortable symptoms that users can experience while using VR systems, including nausea and disorientation (Weech, Kenny, and Barnett-Cowan 2019). Studies have shown, however, that recent advances in VR development with regards to display resolution, frame rates, and interpupillary distance have improved these symptoms, creating a promising future as the technology continues to evolve (Combalia, Sánchez-Vives, and Donegan 2023).
Although there was overall agreement, it is important to consider potential reasons for more negative perceptions and barriers to integration. Perceptions were guarded especially for those without XR for statements regarding accuracy of XR in modeling procedures, the operating environment, and modeling of patient-specific anatomy. Additionally, those in the group who already had access to XR were highly critical when evaluating the accuracy of XR in modeling patient-specific anatomy. This is likely due to the program-specific nature of XR software. As XR technology progresses, there is potential for enhanced integration of patient-specific anatomy, offering improved preparation for complex cases. For instance, Condino et al. created an MR-based simulation for hip arthroplasty using patient-specific 3D models which were derived from computed tomography scans (Satapathy et al. 2023). As everyone’s user experience for procedural accuracy may vary, one particular area of interest lies in the integration of artificial intelligence (AI) with VR. Specifically, the pairing of VR with some of the aspects that AI provides such as machine learning and affective computing can be integrated across many healthcare fields to create an individualized learning experience for each trainee (Combalia, Sánchez-Vives, and Donegan 2023; Satapathy et al. 2023). Additionally, the integration of VR with AI can accelerate the speed and quality of which 3D virtual environments can be programmed, potentially addressing accuracy concerns (Park, Tiefenbach, and Demetriades 2022). Further studies may also evaluate the effectiveness of XR based on training level, as its utility for younger trainees may be particularly useful for arthroplasty, given the lack of available arthroscopic learning resources, while upper-level residents may not receive tactile motor feedback, lessening the perceived value of VR (Kuhn et al. 2024; Pettinelli et al. 2023).
Finally, cost was identified as the largest perceived barrier to widespread integration of XR identified in this study. Of note, there is a growing body of evidence providing reassurance that the costs involved with XR are likely to decrease over time (Bergin and Craven 2023; Longo et al. 2021). As both Mandal et al. and Combalia et al. argue, various technological advances in hardware and software production should lead to decreased future costs (Combalia, Sánchez-Vives, and Donegan 2023; Mandal and Ambade 2022). Additionally, with communal software programs such as “Unity,” programming applications have become increasingly accessible, expanding the potential for future XR developments at a reduced price (Combalia, Sánchez-Vives, and Donegan 2023).
Limitations
This study sought to thoroughly evaluate the perceptions of orthopedic surgery residents on the utility of XR in training, however, it is not without limitations. Inherent to all survey studies, volunteer bias may be present in our data as those with access to XR may have been more likely to respond and have more favorable responses. This in combination with use of the Likert scale could have introduced a response and/or acquiescence bias. The effects of these confounding factors may be more pronounced as there were only 77 responses, 54 of which were complete. Thus, larger studies are required to further elucidate the perceptions of XR among orthopedic surgery trainees. Finally, as the study design was cross-sectional in nature, our results only provide insight into a relatively short time frame, thus longitudinal studies would help understand how perceptions of barriers and accuracy evolve with the advent of newer technologies.
Conclusions
It is clear from the results of this study that overall, orthopedic surgery residents agree that there is a need for surgical training outside of the operating room. Although there was less agreement if XR specifically should be used to fill this demand, trainees agreed that these technologies improved their operative confidence and skill progression. Therefore, these results lay the groundwork for the utility of XR, with further longitudinal studies in large cohorts necessary to further understand the best practices for effective implementation.