Introduction
Healthcare spending in the United States is among the highest in the world, accounting for more than 17% of gross domestic product and reaching $2.3 trillion spent annually (Agarwal, Agarwal, Querry, et al. 2018; Robinson et al. 2012). It is projected to reach 6.2 trillion dollars in annual spending by 2028 (Gardezi, Ottesen, Tyagi, et al. 2021). By the year 2025, combined surgical spending alone is expected to reach $912 billion (Sathiyakumar, Jahangir, Mir, et al. 2014). In the field of orthopaedics, device cost constitutes a large portion of surgical costs, ranging from 30% to 87% of the cost of an orthopaedic procedure (Okike, O’Toole, Pollak, et al. 2014; Wasterlain, Melamed, Bello, et al. 2017; Terhune, Cannamela, Johnson, et al. 2016).
Physicians play a key role in containing healthcare costs, as they influence over 60% of healthcare costs (Gardezi, Ottesen, Tyagi, et al. 2021; Okike, O’Toole, Pollak, et al. 2014; Arliani, Sabongi, Batista, et al. 2016; Johnson, Pinto, Brabston, et al. 2020). As many as 36% of physicians express a great sense of responsibility for helping control healthcare costs (Johnson, Pinto, Brabston, et al. 2020). Despite this, physicians, and particularly surgeons, have been shown to have poor knowledge of supply costs, even within their own field (Agarwal, Agarwal, Querry, et al. 2018; Arliani, Sabongi, Batista, et al. 2016). To date, there is a paucity of information on field-specific awareness of sports medicine related implant costs among orthopaedic surgeons. This study focuses specifically on sports-medicine-related implant cost awareness within a cohort of surgeons who regularly treat sports-related conditions.
The purpose of this study is to determine a baseline awareness of sports-medicine-related implant costs among orthopaedic surgeons. Outcomes of interest include accuracy of estimated costs of various sports-medicine-related orthopaedic implants as estimated by orthopaedic surgeons from various subspecialties, levels of training, and interest in cost-containment. We hypothesize that sports medicine fellowship trained orthopaedic surgeons would more accurately estimate implant and construct costs than their counterparts that did not complete a sports medicine fellowship.
1.1 Materials and Methods
1.1.1. Survey Design
This cross-sectional survey study was determined to be observational and therefore exempt from formal Institutional Review Board (IRB) review. A survey containing images of 10 commonly used, sports-medicine-related implants was sent to included surgeons’ emails. Implant choice was based on a broad scope of practice (such that each surgeon used at least one of the implants represented) and breadth of implant cost to allow for analysis of baseline implant cost under- or overestimation by surgeons. The data was then collected through an electronic data collection software, REDCap (Marblehead, Massachusetts). This survey was tested by a sample cohort to determine clarity of questions and scope of the questionnaire. The sample cohort was also asked to comment on if the survey included pertinent topics such as training/experience, prior involvement in cost negotiation, and routine use of tested implants in practice. The survey was revised based on the comments and feedback of the sample cohort prior to being sent out to the study participants. This process has previously been described for creating an effective original survey (Klein, Hussain, Sprague, et al. 2013).
1.2.2. Study Participants
This study took place in a large metropolitan healthcare system that is affiliated with a private orthopaedic practice and a large university practice with associated residency program. All surgeons listed on the health system website to treat sports-related injuries were invited to participate in the study. Those who did not complete any cost questions on the survey were excluded from the study. Study participants were asked to provide information regarding years of surgical practice, field of fellowship training (if any), involvement in institutional cost negotiations, and importance they place on implant cost in their daily practice. They were then asked to estimate the costs of 10 sports-medicine-related implants, noting the frequency of use of each implant in their practice (Appendix A).
1.2.3. Study Outcomes and Statistical Analysis
The primary outcome of interest for this study was the accuracy of surgeon cost estimates for each implant. The error for each individual response was calculated as the estimated cost minus the actual cost as listed in the institutional charge master database. Accuracy was then expressed in percent error (calculated error divided by the actual implant cost times 100). For easier comparison with previous studies (Okike, O’Toole, Pollak, et al. 2014), estimates within 20% of actual implant cost were considered correct. Statistical analysis was performed using Microsoft Excel (version for Microsoft 365; Redmond, WA) and Intellectus (Clearwater, FL). Specific tests used included Fischer exact tests, independent t-tests, and analysis of variance (ANOVA). Statistical significance was defined as an alpha value of 0.05.
1.2. Results
1.2.1. Study Participant Demographics
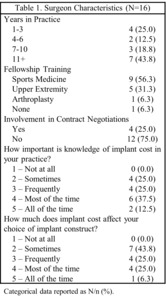
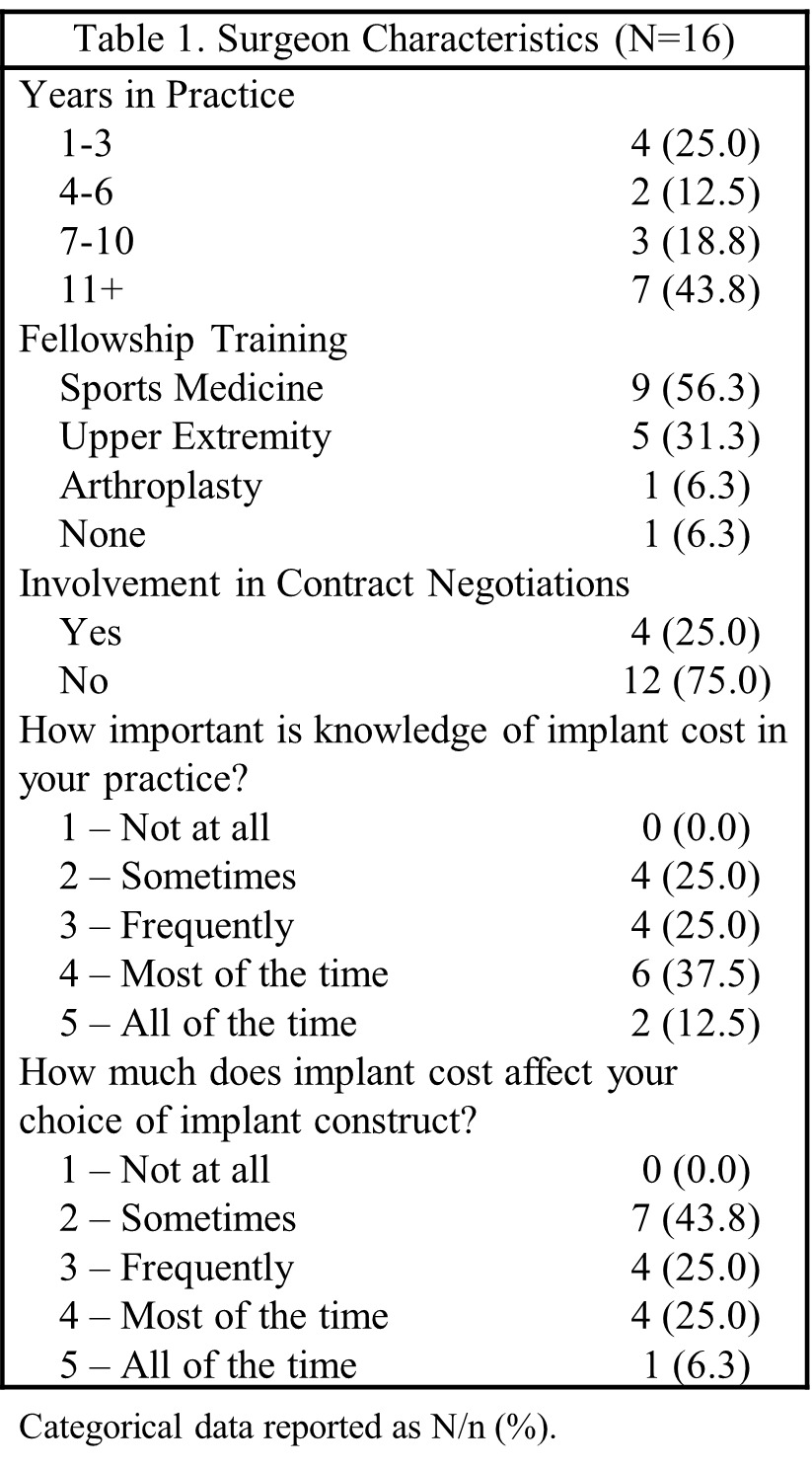
A total of 18 surgeons were invited to participate in the present study, with an 89% response rate (16 out of 18). Of the respondents, 15 completed a fellowship, with more than half (9, 56%) completing a fellowship in sports medicine. Seven surgeons (44%) had completed 11 or more years of surgical practice. Half of the participating surgeons reported that knowledge of implant cost was important in their practice either most of the time or all of the time, but only 5 surgeons (31%) reported that implant cost influenced their choice of implant most or all of the time. Four (25%) participants indicated that they had previously participated in institutional implant cost negotiations (Table 1). Surgeons reported utilizing an average of 4 (Range: 1-7)of the queried implants in regular use in their practice.
1.3.2. Cost Estimation Accuracy
Cost estimates varied greatly across providers regardless of fellowship training. The mean absolute error across all providers was 56.9%. Sports medicine trained participants tended to estimate cost more accurately than their counterparts not trained in sports medicine, although this did not reach significance (mean error: -10.6% vs 29.4%; p = 0.110). Interestingly, those that considered knowledge of implant cost to be important most or all of the time in their practice tended to predict implant costs less accurately than their counterparts who reported that cost knowledge was sometimes or never important (mean error: 60.7% vs 47.9%; p = 0.509). Years of surgical practice, sports medicine fellowship training, and involvement in implant price negotiations had no significant effect on implant cost estimate accuracy.
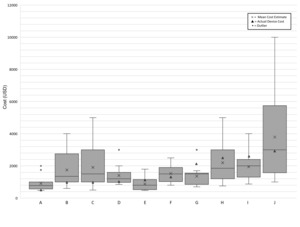
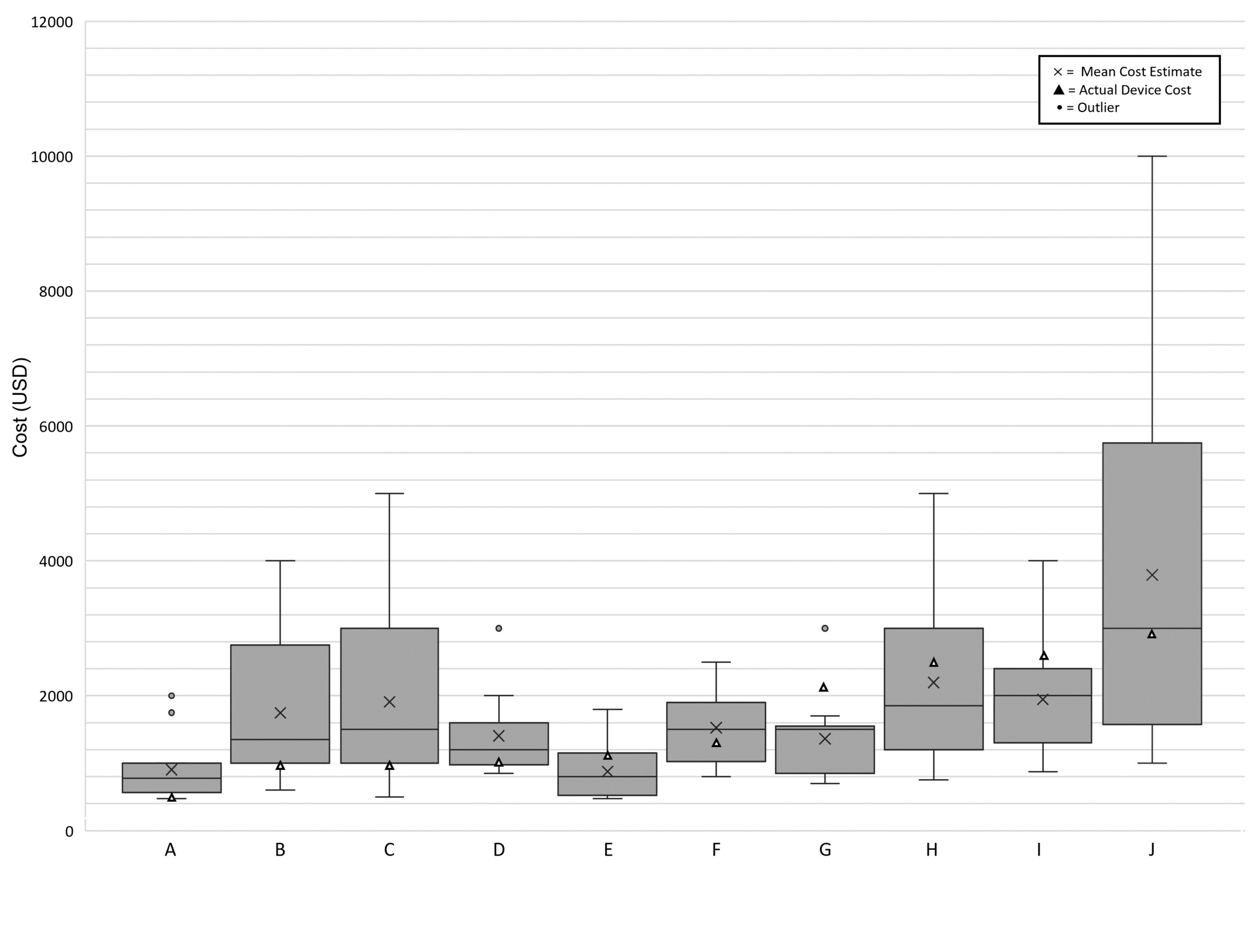
The mean cost of the implants examined in this study was $1709.40 (range: $515 to $2900). Implants costing less than $2000 were more likely to be overestimated than those costing more than $2000 (Figure 1). The largest number of correct estimates (estimated within 20% of actual cost) by any one surgeon was four (40%). This was obtained by two surgeons. On average, surgeons correctly estimated the cost of 2 implants (20%). If the margin of error permitted was increased to 40% error, the largest number of correctly estimated implants was 8. This was obtained by one surgeon. The average number of implants guessed within 40% of their true value by any one surgeon was four (Figure 2).
1.3. Discussion
1.4.1. Primary Study Outcomes
The objective of this study was to determine baseline awareness of implant costs among orthopedic surgeons that perform sports-medicine-related procedures. Eighteen surgeons were queried about surgical training, length of practice, and previous involvement in cost negotiations. They were then asked to estimate the cost of 10 sports medicine related implants. Cost estimates were compared with actual costs as found in the institutional charge master database. These were found to vary widely among all providers regardless of fellowship training, years of experience, and prior involvement in institutional implant cost negotiations. On average, providers’ estimates of implant cost differed by 54.3% from actual implant costs disregarding direction of error (underestimate vs. overestimate). The average number of correct estimates was 2 (range: 0 to 4). Providers who reported that knowledge of implant costs was important in their practice most or all of the time were no more able to accurately estimate implant costs compared to their counterparts who considered knowledge of implant costs to be somewhat or not at all important (60.7 % versus 48.0%, p = 0.5).
1.4.1. Review of Relevant Literature
On average, the absolute error of cost estimates among orthopaedic surgery attendings and residents is 69% when estimating general orthopaedic implant cost. Among attendings alone, previous studies have shown a mean percent error of 59% ± 9%, consistent with the 54% average error found among this cohort of orthopaedic attendings (Streit et al. 2013). Orthopaedic surgeons at all levels of training and practice are reported to correctly estimate within 20% of true implant cost 19% to 35.6% of the time, with equal propensity to over- or under-estimate costs (Okike, O’Toole, Pollak, et al. 2014; Ayoub, Bassett, Seuffert, et al. 2018). Our study demonstrates similar rates of correct cost estimates among orthopaedic surgery attendings, with 23% of cost estimates falling within 20% of the actual implant cost. Additionally, both studies demonstrate undervaluing of high-cost items and overvaluing low-cost items, consistent with the findings in this study (Okike, O’Toole, Pollak, et al. 2014; Ayoub, Bassett, Seuffert, et al. 2018). There was no significant difference in accuracy of cost estimates among the orthopaedic subspecialties, which is in alignment with previous studies that demonstrate no effect of fellowship training on cost estimate accuracy (Arliani, Sabongi, Batista, et al. 2016).
Our study highlights the importance of education around implant cost in the field of sports medicine. Historically, managing physician behavior has proven challenging, however, there has been success lowering surgical costs with the implementation of cost scorecards. Previous studies have employed the use of surgeon scorecards that report costs, including implant cost, postoperatively (Wasterlain, Melamed, Bello, et al. 2017; Brustein, Ponzio, Duque, et al. 2022; Zygourakis, Valencia, Moriates, et al. 2017; Tseng et al. 2020). These studies demonstrated significant cost decreases in implants used by price-aware surgeons as opposed to their price-naïve counterparts (Wasterlain, Melamed, Bello, et al. 2017). Cost variability was found to decrease by 61% among providers with cost reduction up to 43.1% after intervention (Tseng et al. 2020). This pilot study establishes a baseline cost-awareness amongst surgeons that routinely perform sports-medicine-related procedures. Future studies should focus on analysis of physician stewardship regarding implant costs after the employment of postoperative surgeon scorecards in the same cohort. The success of previous such studies provides hope for the future of cost awareness and cost containment in the field of orthopaedic sports medicine.
1.4.3. Strengths and Limitations
This study had many strengths and weaknesses. Despite the authors’ best efforts to involve as many surgeons as possible, the small sample size limits robust analysis of trends in cost estimates. All providers surveyed in the present study were within a single institution in a metropolitan area. As implant costs vary greatly among institutions and availability of cost information to providers is often limited, the data collected is not generalizable to other healthcare systems. One strength of this study is the unique nature inherent to analysis of sports-medicine-related constructs, and the focus on surgeons that provide treatment for sports-medicine-related conditions. This is a pilot study within this cohort of surgeons; therefore, knowledge was not informed by prior cost awareness efforts. This study also acknowledged the effects of previous engagement in contract negotiations, albeit minimal.
1.5. Conclusions
Implant cost awareness is meager at best amongst orthopaedic surgeons in the field of sports medicine despite its critical role in cost containment and value-based care. Our study demonstrates that years of experience, sports medicine fellowship training, and involvement in contract negotiations had no significant effect on implant cost estimate accuracy. There remains great room for improvement in cost awareness in the field of sports medicine.
Acknowledgements
None
IRB Approval
This study was deemed to be exempt by the Institutional Review Board due to its observational nature.


_and_40__(solid)_of_actual_institutional_cos.png)
_and_40__(solid)_of_actual_institutional_cos.png)