Introduction
Osteochondritis dissecans (OCD) is a musculoskeletal disorder that causes defects of articular cartilage and underlying bone (Accadbled, Vial, and Sales de Gauzy 2018). OCD lesions have an incidence of 6-11 per 100,000 person-years which represents a sizable portion of the population (Bruns, Werner, and Habermann 2018; Pareek et al. 2017). OCD affects juvenile and young adult populations, often presenting with activity-related pain. While the specific etiology is unclear, there are a variety of proposed mechanisms including endocrine factors, repeated microtrauma, ischemia, inflammation, and spontaneous osteonecrosis (A. F. Anderson and Pagnani 1997). OCD has been classified in multiple ways, all with some assessment of lesion depth and displacement (Chau et al. 2021). Current treatment options include observation, lesion (or loose body) excision and treatment of the defect with debridement or other cartilage restoration procedure, and open reduction and internal fixation (ORIF) of the fragment (A. F. Anderson and Pagnani 1997). Studies have shown that operative fixation of osteochondral lesions in the knee yield promising results, with up to 90% of cases going on to complete healing (Bruns, Werner, and Habermann 2018).
While OCD lesions occur in multiple anatomical locations, their most common locations in the knee joint are the medial (70%) and lateral (15%) femoral condyles and less frequently in the patella (5-10%) (Zanon, Di Vico, and Marullo 2014). OCD lesions involving the trochlear are very rare, accounting for about 1% of cases (Zanon, Di Vico, and Marullo 2014). These cases are distinct from the osteochondral fractures that can occur in the setting of patellar dislocations and are more commonly seen. Not surprisingly given these numbers, there is very little prior work that focuses specifically on fixation of OCD loose bodies in the trochlea. The one study reporting outcomes of ORIF of trochlear OCD lesions included 16 skeletally immature patients (Price et al. 2020).
The goal of this case series is to report the outcomes following ORIF of trochlear OCD loose bodies with a focus on repair failure, patient-reported outcomes, and post-operative activity level. We hypothesize that loose body fixation results in high rates of healing and good patient-reported outcomes.
Methods
Patient Identification
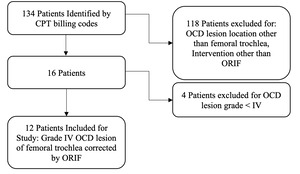
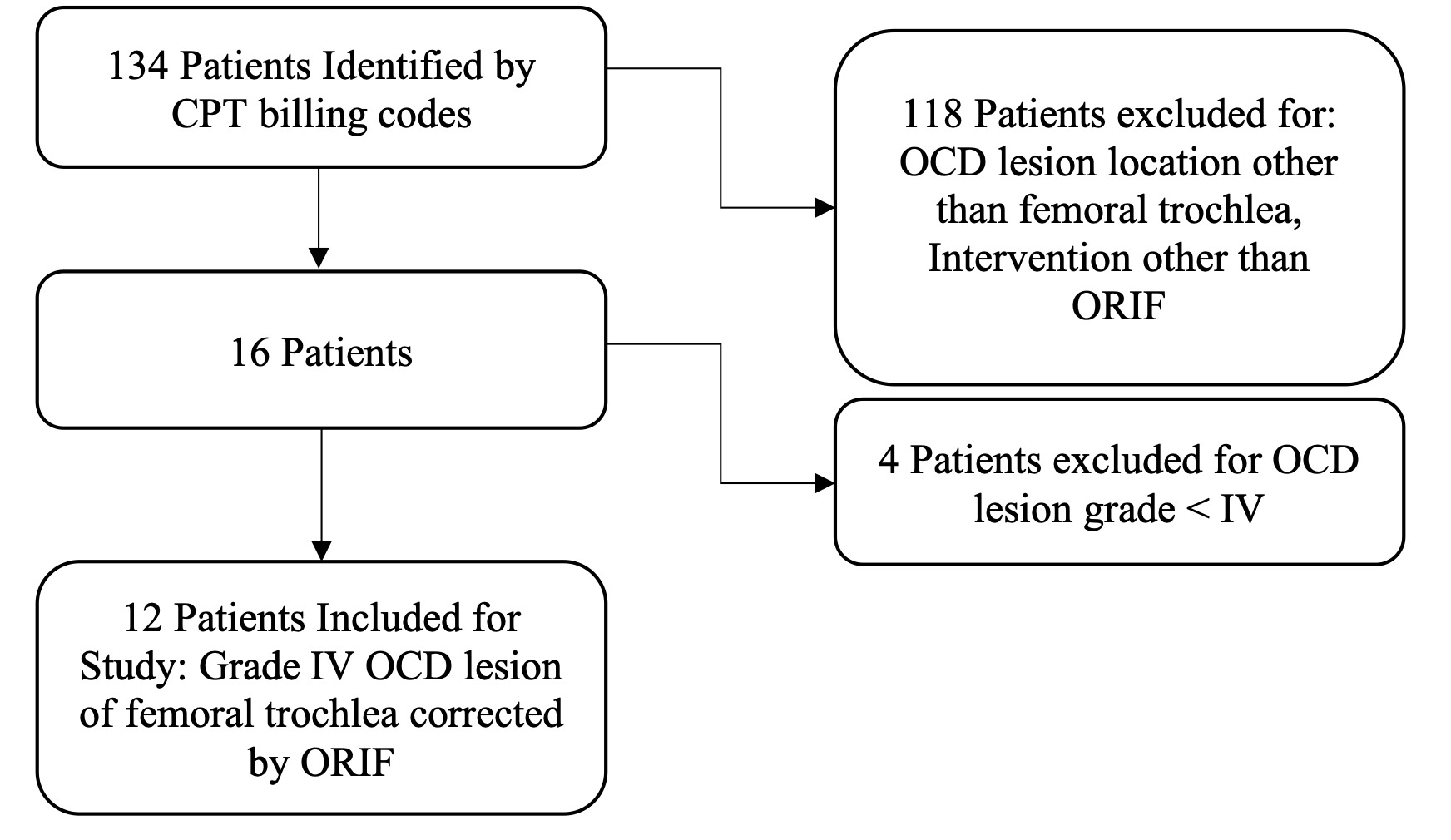
Following institutional review board approval, a retrospective chart review of patients diagnosed with OCD who had undergone surgical intervention for an OCD lesion by the senior author was conducted. Patients were eligible for study inclusion if underwent ORIF of a grade IV (loose body) OCD lesion (Johnson et al. 1990) in the femoral trochlea between 2010 and 2021. Patients treated for defects in other anatomical locations in the knee or with techniques other than ORIF were excluded. To identify qualifying patients, a search of billing records was conducted for relevant CPT codes, which yielded 134 patients. All patient charts were screened against the aforementioned inclusion and exclusion criteria and 12 knees in 12 patients were identified for inclusion (Figure 1). Chart review was undertaken to collect patient demographic and surgical information and to identify documented cases of repair failure.
Surgical Technique
Procedures began with diagnostic arthroscopy to evaluate for any concurrent knee pathology. Upon completion of the arthroscopic assessment, a 5-8cm long medial or lateral parapatellar arthrotomy was created based on patient size and defect location on the trochlea. The base of the OCD lesion was curetted until subchondral bone was encountered prior to fixation. In three cases, autologous bone graft from the proximal tibia was utilized to partially fill the defect prior to loose body fixation. Fixation was achieved with either two or three Lactosorb 2.0 nails (Zimmer Biomet. 2010, Jacksonville, FL.) or two to four ConMed SmartNails (ConMed. 2012, Largo, FL.) of differing length and gauge as appropriate for defect size.
Post-operatively, patients were put into a knee brace locked in extension and allowed to weight bear as tolerated immediately following the procedure. Patients were to use continuous passive range of motion devices for six weeks and underwent physical therapy to help restore joint mobility, achieve effusion control, and restore gait.
Follow-up
Patients were contacted by phone to identify additional cases of repeat surgery on the index knee and obtain patient-reported outcomes data. Fixation failure was defined as failure of any part of the defect to heal at reoperation on the index knee. Patients were verbally administered the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire as well as the Marx Activity Rating Scale (MARS) over the phone by a researcher independent of the surgical team (Collins et al. 2016; Marx et al. 2001; Roos and Lohmander 2003; Roos et al. 1998; Shirazi, Israel, and Kaar 2016).
Statistical Analysis
Summary statistics were calculated for demographic, surgical, and outcomes data, including counts and percentages for categorical data and means and standard deviations for continuous variables. A subgroup analysis based on skeletal maturity at the time of ORIF was performed qualitatively as there were insufficient numbers for a meaningful statistical comparison of outcomes based on skeletal maturity. Statistical analyses were conducted in Microsoft Excel (Microsoft Corp. 2018, Redmond, WA) and R Statistical Software version 4.10.
Results
Twelve knees in twelve patients were identified and included in this case series. Average age at surgery was 17.7 ± 6.4 years old (range, 13-37). 11 of the patients were male and 11 of the patients were Caucasian. Mean trochlear OCD size was 3.20 cm2 (range, 1.69-5.06 cm2) with mean follow-up of 78.9 months (range, 8 – 145) (Table 1). Ten patients were available for telephone follow-up and completed patient reported outcome measures (PROMs) at a mean of 92.2 ± 38.8 months (range, 24-145).
Two failures of fixation were identified in this series. One patient had a recurrence of symptoms 6 years from initial ORIF, which was then treated with a microfracture surgery. A second patient suffered an athletic trauma one year after surgery and was also treated with microfracture. At final follow up, the mean KOOS global score for all patients was 86.8 ± 16.3, symptoms/stiffness sub score 90.0 ± 11.0, pain 91.2 ± 12.1, Functions of daily living 95.5 ± 8.3, Sports/recreation 82.0 ± 23.9, quality of life 75.7 ± 28.6, and a mean Marx activity score of 10.5 ± 4.9.
Subgroup Analysis
There were 5 skeletally mature (SM) patients and 7 skeletally immature (SI) patients included. Mean trochlear OCD lesion size was 2.97±1.05 cm2 in SM patients and 3.37±1.54 cm2 in SI patients with no significant difference noted between groups (p = 0.61) (Table 2). The mean time to follow up in the SM group was 66.2 ± 48.7 months and was 88.0 ± 47.1 in the SI group (p = 0.46).
Failure of fixation occurred in one patient in each group. In the group of 10 patients who completed patient-reported outcomes, scores were generally noted to be lower in the skeletally mature group, but low numbers precluded meaningful statistical analysis.
Discussion
The most important finding of our case series is that ORIF for OCD lesions results in a low reoperation risk and acceptable patient reported outcome measures after surgery.
While there are few prior studies of ORIF of OCD lesions of the trochlea, the results of this study are similar to those reporting ORIF of OCDs more generally in the knee. Prior studies have reported success rates ranging from 75-92% (Johnson et al. 1990; Fokter et al. 2012; Grimm, Danilkowicz, and Shea 2019; Hefti et al. 1999; Magnussen, Carey, and Spindler 2009). Most literature on this topic are other small case series given that the fixation of OCD is uncommon. A recent paper by Price et al. identified 16 patients who underwent surgical fixation of the trochlea (Price et al. 2020). Price et al. reported a mean follow up of 22.2 months and reported a repeat surgery rate for 2/16 patients (12.5%) and the majority of patients returning to sport (Price et al. 2020). The present study reports mean follow up of greater than six years with similar reoperation rate of 2/12 (16.7%) in a relatively active cohort. While our studies differ in their inclusion of stable lesions compared to the present study looking only at loose body lesion fixation, both studies found similarly positive results for operative management of trochlear lesions.
Most other reports to compare our results with are based on fixation of OCDs of the femoral condyle. For example, Fokter et al. reported a success rate of 75% for a cohort of eight patients with mean age 15.3 years and mean long-term follow-up of 14.8 years. Makino et al. reported a success rate of 87% for 14 patients with mean age of 20 and mean follow-up of 4.2 years (Makino et al. 2005). Magnussen reported stable union at 12-week follow-up in 92% of their patients (Magnussen, Carey, and Spindler 2009). Finally, Johnson et al. reported a success rate of 88% at two-year minimum follow-up of arthroscopic fixation with mean patient age of 19 (Johnson et al. 1990). Our results show comparable success rates in a similar group of patients.
Very few prior investigations have reported KOOS scores following loose body fixation. Historical studies report International Knee Documentation Committee (IKDC) and Tegner activity scores or no patient reported outcomes at all. Magnussen et al reported KOOS scores in a series of 12 patients with condylar and/or trochlear defects (Magnussen, Carey, and Spindler 2009). In our case series, higher postoperative KOOS scores were seen in symptoms 90.0, pain 91.2, activities of daily living 95.5, sport 82.0, and quality of life 75.7 when compared to the same scores from Magnussen et al: symptoms 81.8, pain 87.8 activities of daily living 93.1 sport 74.0 and quality of life 61.9. Anderson et al presented a case series of 5 patients who underwent chondral loose body fixation and reported mean KOOS pain score of 91 but sports and recreation function sub-score of 70 (C. N. Anderson et al. 2013). We did find that the present investigation found higher scores in the sports and recreation function subset of the KOOS questionnaire. These differences may reflect a slightly increased (19 vs 17) age in the Anderson study compared to the present one, or differences in athletic activity or location of defect. Englund et al. designated cutoffs for the KOOS sub-scores to define a symptomatic knee for a patient undergoing meniscectomy (Englund, Roos, and Lohmander 2003). Extrapolating these criteria to our series, three patients still had symptomatic knees.
While too small to achieve a meaningful comparison of outcomes based on skeletal maturity at the time of surgery, skeletally immature patients reported higher KOOS scores compared to the mature group. A larger sample size and prospective study would be required to fully investigate this preliminary finding and see if there is a true difference in functional outcomes as measured by KOOS scores based on skeletal maturity.
Limitations
This case series does have limitations. There were only 12 patients identified in this series due to the scarcity of trochlear defects, representing 100,000 – 200,000 person-years (Bruns, Werner, and Habermann 2018). This series is also underpowered with only 12 patients; future studies with a larger sample size and prospective study is required to draw larger conclusions. There were two patients who did not complete patient reported outcomes and patients with lower outcome scores may be less likely to participate. We do not have baseline functional scores on patients, so we were unable to report on change in function. Implant choice did vary across patients in this group and autologous bone graft was used in some but not all cases depending on the size and depth of defect, and this could affect outcomes. Comparative data on fixation approach and implant choice with regards to OCD fixation is limited.
Conclusions
ORIF of loose OCD lesions of the trochlea is associated with a low risk of failure of fixation and acceptable patient-reported outcomes.