Introduction
Distal triceps tendon injuries are rare and commonly undiagnosed (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015; Walker and Noonan 2020). Triceps tendon injuries are the least common of tendon injuries, comprising approximately 1% of all cases (Anzel et al. 1959; Keener and Sethi 2015; Walker and Noonan 2020; Yeh et al. 2010). This injury is more common in active men between 30 and 50 years old, with a 2:1 frequency compared to women. They can also appear in adolescents with incomplete or recent fusion of the olecranon physis (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015). Patients can usually identify the traumatic event that caused the injury. A common mechanism is eccentric loading of a contracting triceps, for example lowering a barbell bench press.
Risk factors include anabolic steroid use, local steroid injection, hyper-parathyroidism (Tsourvakas et al. 2004) and olecranon bursitis (Keener and Sethi 2015; Walker and Noonan 2020). The diagnosis can be made clinically with imaging such as ultrasound only necessary for equivocal cases, such as partial tears (Walker and Noonan 2020). About half of triceps injuries are not initially diagnosed, often as the initial assessment is not performed by an orthopedic specialist (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015). Delayed diagnosis and treatment may lead to poorer patient outcomes (Badia 2020). Whereas complete triceps tendon ruptures require surgical repair, it is not known what the maximum proportion of a partial rupture may be treated non-surgically (Keener and Sethi 2015). We recommend tears greater than 50% width and full depth are recommended for surgical treatment (expert opinion).
Triceps tendon injuries are uncommon and rarely described bilaterally. Here we review the anatomy and biomechanics of triceps injury, analyze the risk factors and describe two cases of bilateral triceps tendon injury and outcomes from a single US center.
Anatomy and Biomechanics
The triceps muscle is pennate and composed of three distinct muscle bellies: long, lateral and medial heads. It is innervated by the radial nerve (C6-C8) and supplied vascularly by deep branches of the brachial artery (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015).
The long head of the triceps has a broad origin at the infraglenoid tubercle of the scapula and inferior glenohumeral joint capsule. The lateral head has a proximal origin from the humerus just lateral to the teres minor insertion extending distally from the lateral aspect of the spiral groove and lateral intermuscular septum. The medial head originates from the humerus distal to the spiral groove and the medial aspect of the intermuscular septum. Distally, the insertion of the triceps tendon can be divided into the central tendon inserting on the olecranon process and the lateral triceps expansion. The central tendon is thicker medially where a distinct rolled edge is formed by confluence of the medial and long head tendons. The deep surface of the tendon is covered by muscle fibers from the medial head. The thickness of the central tendon just proximal to the olecranon tip is 6.8 cm and the olecranon footprint tendon insertion is wide, and dome shaped (Keener and Sethi 2015).
The main function of the triceps is to extend the elbow, along with the anconeus. At the shoulder, due to the insertion of the long head in the infraglenoid tuberosity, it can assist in the adduction and extension of the arm. Importantly, the triceps swiftly loses extension power with shortening from its insertion; biomechanical studies demonstrate that 2 cm of shortening between the triceps origin and insertion causes a 40% loss of extension force (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015; Tom et al. 2014).
Injury mechanism and risk factors
The principal mechanism of injury is a sudden eccentric load applied to a contracting triceps muscle, often seen during weightlifting or from a fall onto an outstretched hand. Less commonly, triceps rupture can be caused by a direct blow (Anzel et al. 1959). Usually, the injury occurs at the level of the tendon insertion into bone; however, musculotendinous ruptures can also occur (Medina Macias et al. 2006; Walker and Noonan 2020).
Most case reports have associated triceps tendon rupture with anabolic steroid use and weightlifting. Professional football players and other contact sports may be at risk for rupture due to their training regimens and the potential for steroid use rather than the contact nature of the sport (Yeh et al. 2010). Local and systemic use of corticosteroids have been associated with triceps rupture: locally causing collagen necrosis and systematically a reduction of the number and organization of collagen fibers. Other associated conditions include olecranon bursitis, hyperparathyroidism, hypercalcemic tetany causing sustained involuntary muscle contraction, Marfan syndrome and chronic kidney disease is associated with elevated levels of parathyroid hormone which stimulates osteoclastic activity and bone reabsorption and could eventually predispose to rupture (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015).
Diagnosis
The diagnosis is primarily clinical (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015). Patients present with pain, swelling and ecchymosis over the posterior aspect of the elbow. A palpable defect proximal to the olecranon confirms clinical diagnosis (Yeh et al. 2010). Usually, full elbow range of motion is present, and posterior pain may be present with terminal flexion motion. Inability to extend the elbow against gravity is a sign of a complete rupture. However, because of the integrity of the lateral triceps expansion complete central tendon rupture often preserves antigravity elbow extension. in some cases. Both partial and full-thickness ruptures have loss of elbow extension power compared with the opposite extremity (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015). A modified Thompson squeeze test, similar to that performed on the Achilles tendon, with proximal squeezing of the arm causing passive elbow extension, has been reported as a potential clinical diagnostic tool (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015; Yeh et al. 2010).
Plain radiographs should be obtained on presentation and include anteroposterior, lateral views of the elbow. The presence of a small avulsion fracture from the olecranon process (flake sign) is pathognomonic of a triceps rupture (Keener and Sethi 2015; Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015; Walker and Noonan 2020; Yeh et al. 2010). Advanced studies such as a magnetic resonance imaging (MRI), computed tomography (CT scan) or ultrasonography (US) are usually necessary to confirm the diagnosis and can give some idea of the chronicity of injury. Both MRI and US can distinguish partial from complete tendon injuries. MRI can be particularly helpful to identify associated soft tissue injuries. The triceps tendon is best visualized on the sagittal images (Keener and Sethi 2015; Walker and Noonan 2020).
Treatment
Management is controversial and should be oriented individually, taking into account both the localization, size of the tear and the patient’s residual active extension force, as well as the comorbidities and functional level of the patient (Keener and Sethi 2015). For example, a partial tear at the tendinous insertion may be managed non-operatively in a debilitated, elderly patient, whereas the same tear may be managed surgically in a highly functioning athlete. Also, healthy seniors usually require normal triceps function for activities of daily living, such as getting out of a chair. In general, any tear implicating approximately 50% of the tendon, are treated non-operatively in a sedentary person; however, in an active person, with the same lesion, surgical intervention may be appropriate. Complete tears are generally managed surgically (Yeh et al. 2010).
Case Reports
The first patient was a right-handed 47-year-old male who works in real estate. He was seen in our Center, presenting with bilateral elbow pain, with a rating 7/10 (evaluated with the 0–10 Numeric Rating Scale NRS) (Boonstra et al. 2016), (table 1). He described the symptoms as aching. The pain started 3 days prior, when he fell while skiing in Colorado. The patient stated he fell onto his extended arms. After the incident he was seen at an emergency room, where he had X-Rays and MRIs taken of both elbows. He mentioned that he had history of mild elbow pain prior to the fall, and he tried stem cells injections, which did not resolve the pain. He stated the left side was more symptomatic than the right. Physical examination disclosed a visible defect at the distal triceps with ecchymosis posteriorly and inferiorly to the olecranon. The patient had a full range of motion at the elbow. Elbow X-Rays did not show a fracture or other abnormality and MRI scans demonstrated full thickness tearing of both triceps tendons with mild retraction.
Due to the nature of the injury, reattachment/repair of the triceps tendon of the involved elbow was advised. The left elbow was treated first as it was more symptomatic and non-dominant side), and the right elbow was repaired three weeks after the left.
The second patient was a right-handed 51-year-old male, self-employed, and an avid weight-lifter. He had mild pain (3/10) at his right elbow. The patient described the pain as intermittent. The symptoms started after a snowboarding accident in Utah, USA, six months prior to visiting our Center. During this time period the patient saw another physician, who wasn’t an orthopedic specialist, who advised against surgery, as the tendon was already too damaged to be repaired. Five years prior to this injury, this patient had a similar injury on his left elbow, whilst snowboarding. He was seen in our Center two weeks after his left elbow injury and treated surgically.
The patient stated he felt that he had no strength in his right arm and was not able to hold himself up off a bed or chair. The patient had a visible defect at the distal triceps, with no restriction of elbow motion. X-rays revealed a soft tissue defect proximal to olecranon. MRI revealed the triceps was clearly avulsed but with modest proximal migration. In this case, surgical repair was also recommended.
Description of surgical technique
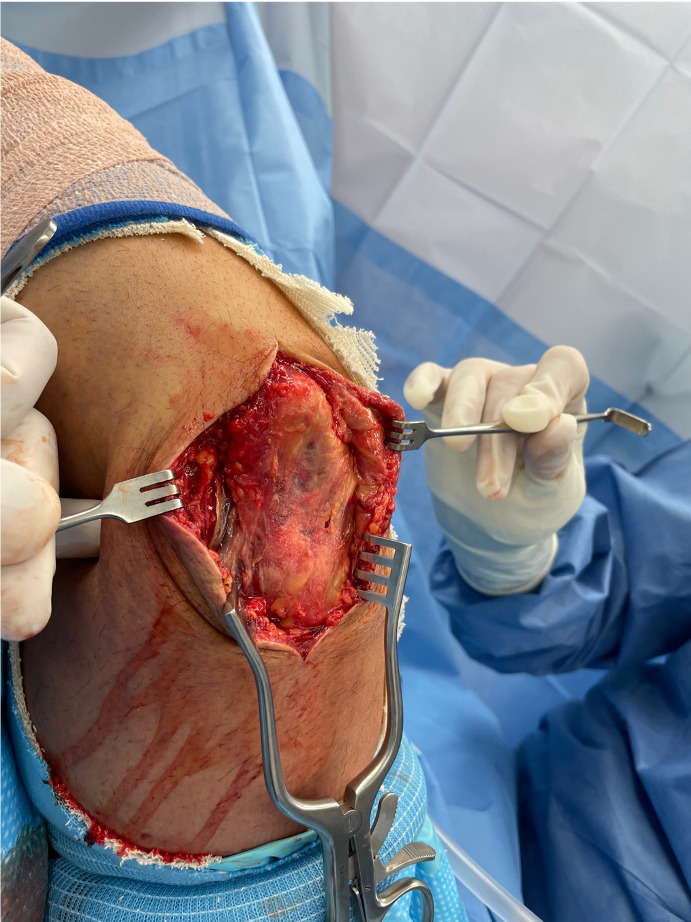
The patient received regional block and intravenous sedation and the patient’s arm prepped and draped in a sterile manner. We prefer to place the patient lateral decubitus position where elbow is placed on an elbow holder, but the position can also be performed in the supine position. HemaClear (Grandville, MI, USA) type tourniquet applied high on the arm, to provide space for the surgical approach. The arm was placed in a limb positioner to aid holding the arm in extension during the surgical repair (Spider2, Smith and Nephew, Watford, UK). The forearm was placed across the chest with the elbow at 90 degrees. A curvilinear longitudinal incision was made over the elbow and distal portion of the triceps (Figure 1). Full-thickness skin flaps were elevated, and the defect was easily identified with fibrosis and scar in the defect, (Figure 2). The scar tissue was excised back to normal tendon tissue. In the chronic case, significant scarring was noted.
Before addressing the triceps, the ulnar nerve was explored, assessed for stability and released in situ. Importantly, the ulnar nerve was released proximally as a triceps tenolysis is required. While protecting the ulnar nerve, scar tissue was released from the medial border of the triceps for 8 to 10 cm proximal to the elbow and then similarly for the lateral triceps border.
Then, the proximal olecranon was debrided to create a bleeding surface for reattachment of the triceps tendon. Two parallel Krackow stitches were passed up each edge of the tendon with a FiberWire Loop suture, grasping the tendon and allowing us to pull it distally (figure 3). Once the sutures were in place, bone tunnels were created in the olecranon using a bone tunneling targeting device (figure 4) (Arthrex, Naples, FL, USA). This device also included a long drill with an eyelet for the sutures pass the sutures and insert them through the tunnel, which was done through a significant portion of the olecranon to create a tunnel with adequate bone around to prevent pullout of the suture, with the elbow placed in full extension to reduce the distance for the triceps to be drawn distally to dock into the olecranon. The HemaClear tourniquet was removed as it would restrict the triceps excursion. The FiberWire sutures are pulled firmly, allowing the triceps to migrate all the way to its insertion site and dock firmly. The area was repaired over and adhered to the triceps to stimulate further healing. The wound was irrigated. At this point, Connective tissue Matrix (CTM) mixed connective tissue allograft fluid was used, which was injected at the repair site. This allowed for growth factors to be introduced and eventually augment the difficult healing process in this particularly challenging clinical scenario of the delayed triceps repair. Subcutaneous closure was done with 3-0 Vicryl, and the skin was closed with 4-0 Vicryl Rapide. The elbow was held in extension and a long arm plaster splint was applied anteriorly.
Postoperative Care
Wounds were assessed at day 2 post operatively, along with range of motion of the hand and wrist. The post operative splint was not removed, and the elbow was maintained at 30 degrees of flexion (table 2).
The second post operative visit was within the first and second week after the surgery. X-rays showed minimal soft tissue swelling. Both patients had the wound properly healed, with no erythema or edema. Both were neurovascularly intact. To protect and stabilize the repair the backslab was converted to a long cast, applied using 2 rolls of fiberglass. After this visit both patients returned for follow up once a month.
In the case of the first patient, it is important to note that there was a three-week difference between the two surgeries. Around eight weeks after the first intervention, the patient began strengthening exercises for the left triceps and further active motion with right elbow. No strengthening on right arm was done for an additional 2 weeks.
Four months later, the patient returned for follow up. He had regained full motion bilaterally and had excellent stability of both elbows. There was minimal discomfort and some residual weakness. X-rays demonstrate the button holds in good position on both the left and right elbows.
Discussion
Comparing to other tendon injuries, distal triceps injuries are relatively rare. Anzel, et al. reviewed more than 1000 cases of tendon injuries and found triceps tendon injuries to be the least common, accounting for less than 1% of the cases (Anzel et al. 1959; Walker and Noonan 2020). In the literature, there are only a few case reports of bilateral triceps rupture. Goodrich et al. reported a case of a patient without risk factors who suffered an injury to both distal triceps with 5 months between episodes. Both injuries were resolved surgically with bone tunnels (Goodrich and Goodrich 2018). The majority of reported cases show injuries that occur simultaneously, regardless of risk factors (Tsourvakas et al. 2004; Desai, Slish, and Allen 2012; Harris, Atkinson, and Moorehead 2004; Sierra et al. 2006). The consumption of anabolic drugs prior to injuries in weightlifters is reported with good results with both conservative and surgical treatment (Harris, Atkinson, and Moorehead 2004; Sierra et al. 2006). Analyzing both of our patients, we note different presentations of the same injury.
On our first patient, the injury occurred on both triceps simultaneously, as he fell with both arms extended while skiing. It’s important to note that prior to the accident, he received local treatment in both elbows (stem cells), since he complained of mild pain. A systemic review by Van den Boom, et al. on the efficacy of stem cell therapy for tendon disorders including tendon rupture included 8 trials and 289 patients (Stein, Stroh, and Schon 2015). All trials had moderate to high risk of bias (2 case series analyzed on the article found that stem cell injections improved patient-reported outcomes in patients with patellar tendinopathy and elbow tendinopathy) concluding that stem cell injections should not be used in clinical practice given the lack of knowledge about potentially serious adverse effects (Sollender, Rayan, and Barden 1998). The use of corticoid injections is much more common in elbow tendinopathy. In most of patients who received repeat injections of corticosteroids, on suspicion of olecranon bursitis, which appears constantly, before the injury and as a prodromal symptom, pain in the footprint of the triceps, may produce tendinosis with tendon weakness or partial tear to a complete rupture. Therefore, it is important to remember the risk of treating inflamed tissues with local steroids injections, especially if they are applied repeatedly and directly onto the tendon, in high demand individuals such as manual works and strength athletes (Medina Macias et al. 2006).
In the case of our second patient, the right elbow injury occurred 5 years later, with a similar mechanism. The second injury was treated 6 months after the accident, after noticing no improvement and continued loss of strength.
Orthopedic misdiagnoses occur frequently, because patients are treated by professionals who don’t have orthopedic training. This is the main reason why many injuries take a long time to receive the appropriate surgical treatment, and consequently, the results are far from expected. That is why we emphasize the early care with orthopedic specialists, we strongly believe that is the key to a better rehabilitation and a prompt labor reinsertion (Badia 2020).
The clinician should enquire about anabolic steroid use, which is common amongst weightlifters (Keener and Sethi 2015; Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015; Walker and Noonan 2020) and may influence tendon healing (Jones et al. 2018). Bilateral presentation in triceps tendon injury is rare. both patients were weightlifters, where anabolic steroid use is common. Both patients declined to answer about steroid use
The use of local and systemic steroids causes collagen necrosis and systemically a reduction in the cross section and organization number of collagen fibrils (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015).
Many techniques have been described to treat distal triceps rupture. No surgical technique has superior clinical outcomes, but each has theoretic advantages. All techniques reattach the torn central tendon to the olecranon. Any disruption of the lateral triceps expansion should be repaired. Recently, modified repair techniques, with either knotless anchors or trans-osseous tunnels have become more popular in order to restore a larger, more native anatomic footprint and improve the mechanical strength of the repair (Keener and Sethi 2015). For chronic cases (6 weeks or more), reinforcement augmentation techniques are commonly used with allograft or autograft using palmaris longus, plantaris or alternatives (Mejia Casado, Carpintero Lluch, and Izquierdo Fernández 2015). In these techniques grafts are sutured with a locked stitch Bunnell, or Pulvertaft in the remnant of the proximal triceps, and are passed retrograde to a transverse trans-osseous tunnel in the olecranon. Alternatively, anconeus muscle rotation flaps or proximal triceps aponeurosis flaps are used in patients with local or systemic risk factors for rupture, retracted or with poor quality tissue.
We advise other clinicians that to achieve a recovery in line with the expectations of an athletic or high-demand patient, the key is a detailed, step-by-step rehabilitation program. When the rupture occurs simultaneously and surgery is performed between both elbows only three weeks apart, recovery is more difficult to predict and can have variable results. In our experience, the key is to follow the patient with close, regular communication with the rehabilitation team. Starting with cast immobilization for the first four weeks, progressing to active flexion and passive extension until week 6. Subsequently, full flexion and extension will continue as tolerated for the first 6 months (Table 2). The return to usual activities will be after the 10th month, which is why it is extremely important to agree on this process with the patient prior to the surgical intervention.
Conclusion
Krackow-type suture configuration in the triceps tendon and parallel bone tunneling is a safe technique with very good results in acute and chronic injuries. CTM injection at the repair site, can augment healing, particularly in chronic cases. We believe that the key to a successful recovery, is careful post-operative rehabilitation, with gradual motion and strengthening.