Introduction
Severity of osteoarthritis (OA) in the knee joint using radiographic findings is a key tool surgeons often use in research, but OA severity grading may also be required to establish necessity for surgical intervention, especially to obtain insurance authorization (Michael, Schlüter-Brust, and Eysel 2010). Joint arthroplasty surgeons routinely utilize the Kellegren and Lawrence (KL) radiographic scoring system to quantify the degree of OA through assessment of anterior-posterior radiographs. The KL classification is based on a simple five-part scale ranging from zero to four (Kellgren and Lawrence 1957). Signs of OA used for grading include joint space narrowing, subchondral sclerosis, cysts, and presence of osteophytes. Furthermore, use of the KL classification has been validated throughout various historically important research studies (SCOTT et al. 1993; Bagge et al. 1992), as well as incorporated into the algorithmic guidelines use by insurance companies to coordinate approval and reimbursement rates for TKA (“Clinical Guidelines CMM-311 Knee Replacement Arthroplasty,” n.d.).
Several studies have investigated whether patient’s preoperative osteoarthritic disease correlates with postoperative success after joint replacement using KL classification and common patient reported outcomes scoring systems. The current literature suggests more severe KL grades correlate with better postoperative outcomes. For example, Valdes et al (Valdes et al. 2012). and Keurentjes et al (Keurentjes et al. 2013). showed that patients with severe OA have significantly better postoperative improvement and recovery after their joint replacement than patients with mild OA- both assessing total hip and knee replacements. Similarly, Dowsey et al (Dowsey et al. 2012). found that patients receiving TKA who had less severe OA at their preoperative assessment had more pain postoperatively than patients with severe OA. In contrast to the previously mentioned studies, Tiblbury et al (Tilbury, Holtslag, Tordoir, et al. 2016). did not find a meaningful correlation between preoperative OA severity and postoperative pain in patients receiving TKA. The latter study postulated that non-radiographic, clinical symptoms may hold greater weight in determining appropriate candidates for surgery than radiographic OA severity (Tilbury, Holtslag, Tordoir, et al. 2016), which invites the question of whether high KL grades are necessary in order to move forward with TKA.
Additionally, use of specific arthroplasty techniques may affect the results of studies that are comparing patients initial OA severity and postoperative reported outcomes. Kinematic alignment (KA) is an arthroplasty technique based upon the principle of restoring the patient’s native pre-arthritic alignment of the distal and posterior femoral joint lines and the proximal tibial joint line (Riley et al. 2018; Keshmiri et al. 2018; Blakeney et al. 2018). Therefore, using kinematic techniques versus other mechanical alignment techniques may affect the previously mentioned findings that more severe KL grade correlated with better postoperative outcomes scores than patients with milder KL scores.
The purpose of this study was to investigate whether preoperative osteoarthritic KL grades correlated with non-inferior postoperative outcomes after kinematic alignment medial-pivot (MP) TKA.
Methods
Patient Cohort
A total of 168 patients previously enrolled in a prospective study who received MP TKA using a kinematic surgical technique between 2018 and 2020 were included in this review. Institutional Review Board approval was obtained, prior to patient chart review. Patients were included in this review if they had at least two years of follow up records including chart notes, patient reported outcome records, and radiographs. Patients were binarized into two cohorts primarily based upon their preoperative Kellgren-Lawrence OA grade of the knee joint: patients receiving KL grades of 1 or 2 and patients receiving KL grades of 3 or 4 were grouped together for subsequent postoperative analysis. Secondary analysis using Kellgren-Lawrence OA grades for the patellofemoral joint were assessed as well. There were 12 patients with low-grade KL but high-grade PF who were excluded from our comparative analysis. As this paper is only focusing on tibiofemoral joint OA, we excluded patients which were only affected by high-grade patellofemoral OA, and who theoretically could have been treated with either a total knee or an isolated patellofemoral arthroplasty. Conversely, subjects with high-grade TF OA, but low-grade PF OA were included in the analysis.
Radiograph Measurements
A complete radiographic series was completed on every subject at the preoperative and one-year postoperative visits consisting of full-length (hip to ankle) and standard (14" x 17") weight-bearing anteroposterior (AP) radiographs, as well as lateral knee and sunrise view radiographs. Patients were given KL grades of the knee (tibiofemoral) and patellofemoral joints using the preoperative 14" x 17" AP radiograph and sunrise PF view, respectively. Each radiograph was scored using the KL five-part scale. Any subject with low-grade TF KL also underwent a standing posteroanterior (PA) 30º flexion view, to further assess the TF KL grade. The association of OA grade and radiological findings are detailed in Table 1. Independent assessment of KL grades was completed by two reviewers (BC, BJ) who were medical students thoroughly trained by the senior author. Inter-reader reliability between observers was evaluated using intra-class correlation (ICC) and resulted in an agreement score of 0.72. Discordant evaluations were resolved by consensus with reviewers and the senior author and surgeon, and subsequently updated for final analysis.
Operative Technique
Surgeries were performed by a single surgeon (DFS) using an identical, unrestricted kinematic alignment surgical technique. This technique has been previously discussed in literature, [26] but in brief, this technique consists of adhering to the kinematic alignment philosophy using manual instrumentation, medial parapatellar arthrotomy, measured resection, intramedullary femoral and extramedullary tibial alignment, and posterior referencing without computer-assisted orthopaedic surgery. Tourniquet inflation to 300 mm Hg was used in all cases prior to incision and deflated prior to closure and before femoral, tibial, and patellar components were cemented. Components cementing was completed on all devices using a surface-cementing technique and carbon-dioxide lavage with medium-viscosity Simplex P cement (Stryker, Kalamazoo, MI, USA). The femur was positioned in neutral position in relation to the femoral condyles and adjusted depending on cartilage and bone less. The tibial slope angle and proximal tibial varus were individually matched accounting for tissue loss in the attempt to mimic the patients natural, kinematic prearthritic joint line. Ligament releases beyond the creation of a medial soft-tissue sleeve during the initial exposure were performed only in the presence of a significant valgus-flexion deformity.
Statistical Analysis
An electronic data capture and analysis system (Ortho Research Master®, Spokane Joint Replacement Center Inc., Spokane, WA) was utilized to perform all data analysis using single factor analysis of variance and Student’s T-Test with a significance level of p≤ 0.05.
Results
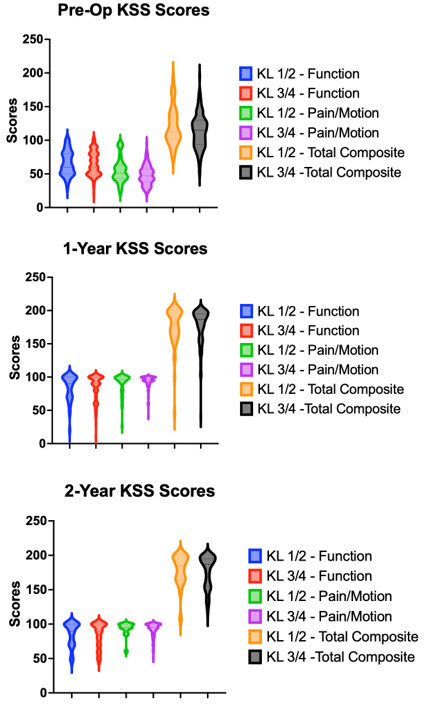
Patient demographics are displayed in Table 2. There were no significant differences in age or BMI. We did not have any patients in our cohort who had a tibiofemoral KL grade of 0 or 1. There were no significant differences in range of motion extension or flexion between the high-grade OA or low-grade OA groups, accounting for both the KL grades of the tibiofemoral joint and patellofemoral joint, at 1-year or 2-year post-arthroplasty. We did not observe significant differences between KSS function, KSS total composite, KSS pain-motion and FJS at one- and two-years post-arthroplasty between high- and low-grade OA patients (Table 3). There was a significant difference in pre-operative KSS Pain scores between the two groups with the low-grade cohort receiving a higher score: 22.3 versus 11.8 (p= 0.03). Similarly, the low-grade cohort had a significantly better pre-operative KSS Pain-Motion scores compared to the high-grade cohort: 60.6 versus 46.4 respectively (p= 0.008). These significant differences were not found to persist at subsequent follow-up appointments (Table 3). All functional out comes are listed in Table 3 and displayed in Figure 1.
Discussion
The goal of this paper was to assess whether TKA outcomes differed in patients with varied severity of preoperative OA. This retrospective single center study observed that patients in both the low-grade and high-grade OA groups had clinically significant improvements preoperative to postoperative. However, contrast to current literature, more severe radiographic OA preoperative did not associate with improved outcomes after two years of follow up. Furthermore, in context of the minimal clinically important difference (MCID) for the Knee Society Scores after TKA, there were no clinically significant differences between low- or high-grade KL groups after two years of follow up (Figure 3). Although inconsistencies and discrepancies have been shown in which the MCID values are derived (Deckey, Verhey, Christopher, et al. 2022), Lizaur-Utrilla et al (Lizaur-Utrilla et al. 2020). established that patients with an improvement of nine to ten points for KSS associated preoperative to postoperative scores had evidence of a clinically important change.
Regarding patient prioritization of TKA, surgical candidates have been historically selected based on a combination of radiographic OA severity, pain, and disability. However, waiting until a patient’s radiographic OA severity has reached end stage may result in poorer outcomes as patient’s overall health and lower extremity strength have likely decreased as a result of their osteoarthritic joint (Gossec, Hawker, Davis, et al. 2007). There is conflicting evidence between the correlation of low-grade OA, demonstrated by the absence of major radiological changes, and improved patient reported outcomes after TKA. A meta-analysis of 29 studies on the association between increased postoperative pain/dissatisfaction after TKA and radiographic OA found that patients with mild radiographic OA (KL < 3) were more likely to have dissatisfaction and increased postoperative pain compared to patients with severe radiographic osteoarthritis (KL 3) (Shohat, Heller, Sudya, et al. 2022). The studies included in this analysis considered a variety of patient reported outcomes and functional scores, and in total, four out of 24 studies indicated that there was no correlation between radiographic grading and functional outcomes postoperative in at least one scoring category. Additionally, Valdes et al. (Valdes et al. 2012), Keurentjes et al. (Keurentjes et al. 2013), and Dowsey et al (Dowsey et al. 2012). have all reported results that contrast the findings shared in this study. The latter studies generally found better outcomes in TKA patients who had severe OA. In contrast, Perry et al (Perry et al. 2015). compared a small, matched cohort of patients with severe vs minimal radiographic OA undergoing TKA and found pain relief, overall satisfaction and function were similar between groups after five years of follow-up. Tilbury et al (Tilbury, Holtslag, Tordoir, et al. 2016). showed comparable findings in terms of TKA patients, but found patients undergoing total hip arthroplasty tended to have better outcomes if they had more severe preoperative radiographic OA.
Dossec et al. (Gossec, Paternotte, Maillefert, et al. 2010), investigated if self-reported pain and function levels could identify patients with mild OA whose surgeons recommend them for TKA. They found the level of physical symptoms were predictive of future TKA. Thus, patients with severe physical disability and limited functionality should be considered for TKA despite potentially having radiographic OA that is non-indicative of a TKA. Following FDA determination of medical necessary TKAs, many insurance providers require KL-OA grades 3-4 on top of debilitating pain that has not responded to conservative treatment for authorization joint replacement (“Medical Policy (7.01.550) Knee Arthroplasty in Adults” 2022). In our study, patients with debilitating pain due to their OA that had not responded to other treatment were treated with a TKA regardless of radiographic OA grade. The successful return of function in all patients suggests that KL grade scoring should not be as heavily weighted in the decision making of surgical readiness. Candidacy for TKA should consider weighting the factors of pain, loss of range of motion, functional losses in actives of daily living, and overall disability more heavily or of similar value as OS severity (van de Water, Leichtenberg, Nelissen, et al. 2019).
When in direct comparison with the results of the aforementioned studies, it is difficult to draw meaningfully conclusions from this study. Cohort comparisons between studies are difficult due to factors that may contribute to worse or better outcomes such as old age, BMI, socioeconomic status, a lower level of education, and even surgical techniques (Gossec, Paternotte, Maillefert, et al. 2010). A notable difference between this study compared to the current literature is the kinematic technique used in each patient’s arthroplasty. To our knowledge there has not been a study evaluating the correlation between preoperative radiographic OA scores to postoperative outcomes solely using a kinematic alignment (KA) technique.
The advantage of KA-TKA is the utilization of patients’ native joint lines during reconstruction with the aims to restore pre-arthritic knee orientation (Sappey-Marinier, Pauvert, Batailler, et al. 2020; Nisar et al. 2020; Calipered Kinematically Aligned Total Knee Arthroplasty : Theory, Surgical Techniques and Perspectives 2021). This philosophy promotes implant design adapted to patient-specific physiological kinematics of the native knee as compared to mechanical alignment that favors a neutral alignment (Keshmiri et al. 2018; Risitano et al. 2020; MacDessi, Griffiths-Jones, Chen, et al. 2020). As KA focuses more on restoring and accommodating the patient’s individual knee, KA has been shown to correspond with functional outcomes favored in comparison to mechanical alignment. Additionally, previous studies indicate improved recovery in postoperative KA patients regarding ROM, function, and a 97.5% 10-year survival of prostheses (Weber and Gollwitzer 2021; Rivière et al. 2017). The indication that preoperative pain scores have a larger effect on postoperative outcomes compared to knee OA supports the efficacy of KA in patients with both low- and high-grade OA reporting higher pre-op pain (Maxwell and Gwo Chin 2017). With the objective of KA-TKAs focusing on adapting to the patient-specific anatomy for enabling higher functionality outcomes and faster recovery, it is consistent with the findings of this study that both low- and high-grade OA patients experienced comparable functional outcomes.
A potential draw back from this study is the total follow up time of two-years. Long term follow-up with component survivorship is required to ascertain meaningful clinical differences. Secondly, our small cohort size affects the significance of our results. Larger, more robust patient cohort size would be able to determine the relationship more definitely between preoperative OA disease and long-term postoperative outcomes. Lastly, measurement of radiographic OA was performed by two non-clinicians which could reduce clinical validity despite having high inter-rater correlation. Additionally, the KL classification system has been observed to be consistent between clinicians and trained non-clinicians, with non-clinicians having an ICC range from 0.56 to 0.85 indicating substantial agreement between observers (Klara, Collins, Gurary, et al. 2016).
In conclusion, this study indicates that among patients receiving KA-TKAs, the severity of preoperative OA did not correlate with differences in functional outcomes. Total joint arthroplasty candidate selection is a nuanced process; however, we believe that weighting patient factors of functional disability and preoperative pain are important proxies and should be considered of equal value to radiographic OA severity.