Introduction
In the United States, hospital care expenditures were 1.3$ trillion in 2021 and are projected to increase 43% by 2031 (Centers for Medicare & Medicaid Services 2023). The rising healthcare costs and the push for value within medicine are driving healthcare provider initiatives to decrease unnecessary costs and improve efficiency while maintaining superior patient care (Healey, El-Othmani, et al. 2015; Healey, Peterson, et al. 2015). The operating room (OR) has become a primary target for improvements due to both its role in generating revenue for hospitals and its potential for excessive expenditure. ORs account for approximately 35-40% of hospital costs and 60-70% of revenue (Schouten et al. 2023), with operational costs recently reported around $36 USD/minute (Childers and Maggard-Gibbons 2018) up to $113 USD/minute in prior publications (Ting et al. 2012).
The causes of OR inefficiency are diverse and range from personnel availability and surgical scheduling to unstandardized operative workflow and OR turnover (Lee, Ding, and Guzzo 2019). Although a large volume of research has been conducted to address these inefficiencies, there still exists considerable room for improvement that includes all stakeholders and aligns metrics across functions (Schouten et al. 2023). While pre- and post-operative factors (such as patient tardiness and patient-provider communication, respectively) also influence OR performance, Part 1 of this narrative review aims to synthesize the existing research on the factors that directly impact activities occurring pre-operatively and the resulting impact on efficiency. Additionally, it will discuss the results of studies employing existing technologies to address these issues and identify opportunities for future technologies to further impact OR efficiency.
Defining Efficiency
The technical definition of efficiency as the output produced per unit of labor or capital (Palmer and Torgerson 1999) is not applicable to ORs due to variations in revenue, surgical durations, and resources (Charlesworth and Pandit 2020; Oh et al. 2011). Past studies have used a variety of metrics to measure OR efficiency, including procedure cancellation rate, first case start time, OR utilization, percentage of unplanned closure, case duration accuracy, operating room turnover time, excess staffing costs, and off hours surgery (Lee, Ding, and Guzzo 2019; Fixler and Wright 2013). However, focusing on one metric alone can lead to unexpected results and may negatively affect systemic efficiency (Schouten et al. 2023; Charlesworth and Pandit 2020). For example, under-booking the OR will lead to less off-hour surgeries and same day cancellations but could potentially decrease OR utilization (Charlesworth and Pandit 2020). To account for these discrepancies, Pandit and colleagues (Charlesworth and Pandit 2020; Pandit, Westbury, and Pandit 2007) proposed an elegant yet simple definition: the optimization of OR utilization without excessive unused time or over-time. OR utilization efficiency can be operationalized using the equation proposed by Pandit et al (Pandit, Stubbs, and Pandit 2009). wherein the fraction of scheduled time used (fraction of scheduled time – fraction of overrun) is multiplied by the fraction of scheduled operations completed.
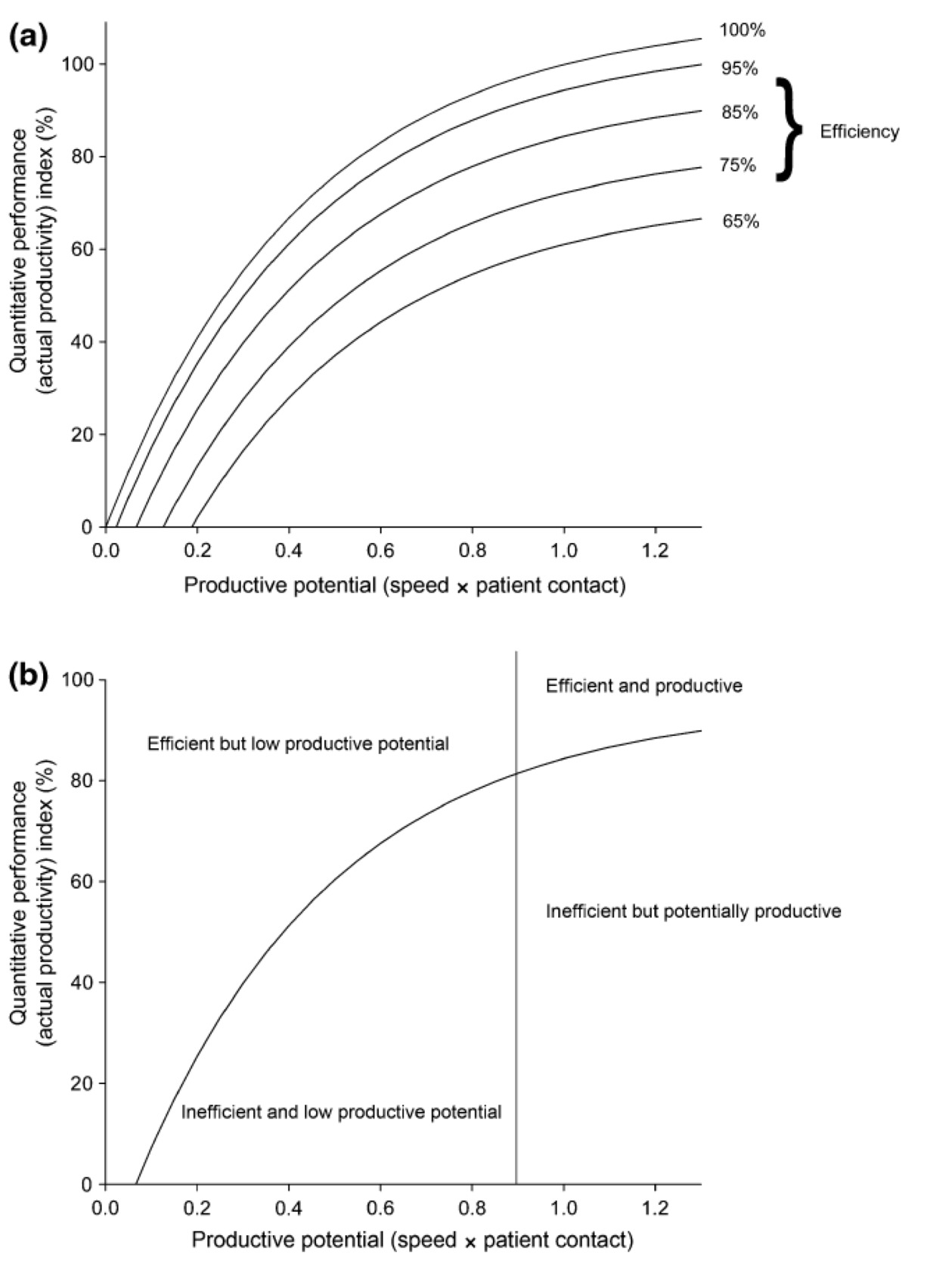
Further work by Pandit and colleagues suggests that the greatest gains in OR efficiency are realized by first optimizing OR utilization efficiency and then maximizing OR productivity by reducing operative (wheels in to wheels out) and gap times (time between patient entering recovery and next patient receiving anesthesia) (Charlesworth and Pandit 2020; Pandit, Stubbs, and Pandit 2009). Thus, the most efficient ORs occur when institutions accurately estimate workload capacity and surgeons/staff minimize wasteful and/or unnecessary tasks (Pandit, Stubbs, and Pandit 2009) (Figure 1):
Pre-Operative Activities Effecting Efficiency
Operating room utilization
Perhaps the largest opportunity to drive operating room efficiency is to improve the organization and scheduling of operating lists. Presently, the elective surgery cancellation rate ranges from 10% to 40%, depending on the size and type of hospital (Adugna et al., n.d.; Sarang et al. 2022). Poor organization of OR schedules, resulting in operative overrun and late starts, is the primary cause of elective surgery cancellation (Koushan, Wood, and Greatbanks 2021) and responsible for 20% to 78% of surgery cancellations (Adugna et al., n.d.; Koushan, Wood, and Greatbanks 2021; Yıldız Altun et al. 2020; Talati et al. 2015). Additionally, up to a third of operating schedules may be under-booked, resulting in a waste of valuable resources (Pandit and Carey 2006). It is thus essential to improve organization and management of operating schedules in order to optimize OR utilization and reduce cancellations (Charlesworth and Pandit 2020).
Traditionally, OR scheduling relied on time blocks allocated to surgeons, surgeon’s case duration estimates, or mean surgical times from databases (Dexter et al. 1999). However, these methods have proven inaccurate, with surgeons correctly estimating operating times only about 26% of the time, resulting in in overbooking ORs 42% of the time and under booking 32% of the time (Laskin, Abubaker, and Strauss 2013). Similarly, setting the operating schedule according to mean surgical times is sufficiently accurate only 13 to 25% of the time, resulting in 50% to 65% of schedules over booked and 10% to 37% schedules under booked (Pandit and Tavare 2011; Proudlove et al. 2013).
To address this, studies have developed algorithms incorporating mean surgical times, standard deviations, surgeon’s estimates, and patient characteristics (Levine and Dunn 2015). For instance, an algorithm developed by Pandit and colleagues (Pandit and Tavare 2011), which incorporated mean surgical duration, pooled standard deviation, and acceptable limits for over-and under-utilization, was shown to appropriately book approximately 76% of OR schedules. Another model based on lognormal surgical duration means, duration variance, and surgeon-specific variance significantly reduced over-and under-reserving per case by approximately 10 and 12 minutes, respectively (Stepaniak et al. 2009).
Machine learning to optimize utilization
Traditional algorithms for predicting surgical durations require significant human input and constant adjustment. In contrast, machine learning, a subset of artificial intelligence (AI), can analyze large datasets and improve task performance without explicit programming (Brown 2021). The use of machine learning to predict surgical duration has grown significantly over the past decade and shows great potential to improve OR scheduling and utilization (Bellini et al. 2019). Studies have demonstrated that machine learning models, using variables such as diagnoses, procedures, and surgeon’s experience, can outperform current estimation practices by as much as 50%, potentially saving up to 5,000 minutes of OR time over the course of two months (Abbou et al. 2022; Huang et al. 2020).
Due to the necessity of detailed patient data, implementation of many machine learning models is limited as backlogs may occur when patient information is missing. Models using pre-operative variables have shown promising results, with one study reporting accurate prediction of surgical time within 10 minutes for 50% of the cases sampled and to result in less than 10% overtime for 73% of the cases sampled (Chu et al. 2022). On the other hand, wide variation was reported between departments, suggesting that the model could be fine-tuned by department for further accuracy.
Digitization of data acquisition
In 2004, a convention of operating room (OR) experts identified the need for “smart” scheduling of OR resources and enhanced data acquisition and surgical informatics (Cleary, Chung, and Mun 2004). Nearly two decades later a second convention of OR experts concluded that many of the challenges associated with OR data acquisition, digitization, storage, and actionability still exist (Maier-Hein et al., n.d.).
Data as simple as timestamps is actionable (Moskovitch et al. 2019), and while machine learning models may address the need for smart scheduling, their accuracy is limited by the quality of the data available. Hospital staff are regularly expected to provide direct care and simultaneously record data associated with the details of the care, which may result in electronic health records that are biased and not suitable for many research questions without accurate timestamps (Agniel, Kohane, and Weber 2018). Manual data recording by hospital staff, such as timestamping, is prone to errors due to stress (Brabrand, Folkestad, and Hosbond 2011), relative perceptions of elapsed time (Ismail, Bin, and Seow 2019), unsynchronized clocks (Cruz-Correia et al. 2009; Ferguson et al. 2005), retrospective recording errors and digit preferencing (Bennett and Wakefield 2001; Locker and Mason 2006; Phelps et al. 2017), and random errors (Ferguson et al. 2005; Bennett and Wakefield 2001; Locker and Mason 2006), all of which are exacerbated by the recoding of large numbers of events (Kaye, Mancini, and Truitt 2005).
The digitalization of data recording systems has the potential to eliminate many errors and biases inherent to human timestamping (Goodwin et al. 2022) and has been shown in preliminary reports to improve accuracy and precision (Bottani et al. 2023). Digitization that enables direct data recording with minimal human interference may also reduce medical staff workload, leading to more cases and patient-centered care (Engle et al. 2021; Kwame and Petrucka 2021). A study by Agnoletti and colleagues (Agnoletti et al. 2013) demonstrated the potential of timestamped data to increase OR efficiency. OR staff were provided with personal digital assistants (PDAs) to timestamp various stages of patient care. The data was then analyzed by an operating room management system (ORMS), resulting in an 8% increase in raw OR utilization, reduced cancellations, and a 7% reduction in overtime. While this study shows the potential for timestamped data to improve OR efficiency, it does not automate data acquisition, and instead places an additional burden on OR staff to interact with the app to timestamp, scan, and record data.
The concept of a smart OR that automatically collects and transmits data was proposed as early as 2007 by Agarwal and colleagues (Agarwal et al. 2007). In 2014, Garbey and colleagues (Garbey et al. 2015) developed a smart OR that automatically timestamped various stages of patient care. The data collected allowed researchers to identify inefficiencies and their root causes, demonstrating the potential of automatic data collection to enhance OR scheduling and utilization. While these findings are encouraging, wide adoption of the system may be limited by the number and potentially cumbersome placement of sensors and motion detection cameras. The advancement of AI, including image recognition, may allow for a single unit to accomplish these tasks without interfering with OR flow. Available technologies and services capable of data capture and analytics need to be considered individually (Table 1).
Conclusions
Over the past decades a high volume of research has been conducted to identify the causes of, and solutions to, operating room inefficiencies. Of these, an efficient scheduling system is crucial for resource utilization and reducing delays. Although the factors contributing to OR inefficiencies are multifactorial, many are predictable and avoidable with quality data and appropriate analytics. Many of the studies referenced within this review demonstrate the potential to use actionable data to improve OR scheduling. However, nearly all the studies increased administrative workload. The adoption of technologies for automated data capture and advanced analytics could help alleviate this burden, enabling OR staff to concentrate on patient care and procedures, and providing stakeholders with actionable data to identify inefficiencies and refine processes. As this review has focused on pre-operative process improvement, Part 2 of this article will discuss intra- and post-operative opportunities for efficiency gains.