Introduction
Blood derivatives are increasingly used to modulate the intra-articular environment, allowing the reduction of inflammatory distress and stimulating anabolism in different tissues. Platelet rich plasma (PRP) is a simple, low-cost, and minimally invasive way to obtain a natural concentration of growth factors and bioactive molecules (Filardo et al. 2021).
Platelet rich plasma has been used in a variety of medical fields, with the aim of stimulating tissue healing through platelet derived growth factors and other bioactive molecules and cytokines. These can stimulate growth and cellular proliferation, tissue regeneration and collagen production (Christin et al. 2022).
The use of biological agents including PRP and mesenchymal stem cells (MSCs) in orthopaedics has increased exponentially over the last few years due to its autologous nature, supposed effectiveness and lack of side-effects (Shahid and Kundra 2017).
Driven by the possibility of delaying the progression of knee osteoarthritis (KOA) with positive results, mainly in the reduction of pain and improvement of the knee function, the authors included PRP injections in the hospital outpatients practice as an alternative to more traditional intra-articular products, such as corticosteroids and hyaluronic acid (HA), in 2019.
Good results have been reported in multiple studies using PRP in KOA when compared to hyaluronic acid, other intra-articular injections and placebo (O’Connell, Wragg, and Wilson 2019).
In this paper, the authors review the first 21 patients treated with a single PRP injection in the outpatient clinic using a commercially available PRP kit and evaluate the initial results related to reduction of pain and improvement of functional status at one, four and eight weeks and compare these results with the results after four years from the injection, using the visual analogic pain scale and the Lysholm questionnaire scores.
Method
This is a retrospective and prospective longitudinal work in which the authors reviewed the charts of the first 21 patients treated with a single PRP injection to the knee and then reevaluated all patients after four years from the injection, in order to assess the short term and long term results of this injection.
A written informed consent was obtained from all patients. The paper was approved by the hospital Institutional Review Board. The work was made in accordance with Helsinki’s Declaration for research in human beings.
All patients had previous weight bearing x-rays documented Kellgren-Lawrence (Kellgren and Lawrence 1957) grade 3 knee osteoarthritis (KOA).
At baseline, personal information (age and gender) and grade of KOA were recorded. Prior to the first injection, all patients were evaluated and none declared the use of medications that could modify the action of the platelets (anticoagulants or plaquetary antiaggregant drugs). No patient had a corticosteroid injection in the six months prior to the PRP injection.
Prior to PRP injection, all patients were followed by their general practitioners and had had pain killers, physiotherapy schemes and common conservative treatments.
Our initial approach was to evaluate knee pain before the injection in accordance to the visual analogic pain scale (VAS). We evaluated the patient’s functional status in accordance to Lysholm questionnaire, in which one can evaluate pain in daily activities and function in common daily situations.
All patients were followed up in weekly intervals and VAS was repeated in the first week, fourth week and in the eighth week after injection. Lysholm questionnaire was repeated in the eighth week after the injection.
After four years from the injection, we called all patients to a new appointment in order to reassess them with VAS and Lysholm questionnaire.
The authors used the Zimmer Biomet GPS3 kit™. All patients received only one injection of 6mL PRP to the painful knee. When there was pain in both knees, the patient opted for the most painful one to receive the injection.
PRP was prepared as follows: a 60mL blood sample was collected from each patient and centrifuged with GPS3 system™ for 15 minutes at 3200 rpm. This could generate 6mL of pure PRP to be injected. According to data on file from the manufacturer, this system provides 90% of recovery of platelets and concentrates platelets to 9.3 times over baseline providing an output of 6 mL of PRP.
The injection was made in an outpatient basis with aseptic technique in order to avoid injection site infection. The site of injection was located in the lateral soft spot of the knee, similar to the lateral portal in knee arthroscopy, with the knee flexed 45 degrees. This anatomically guided procedure does not require the use of ultrasound.
Any complication or discomfort by the patients was noted. All patients received a written recommendation to avoid weight bearing with the use of crutches in the first two weeks after the injection.
Active flexion-extension exercises were recommended. Since the goal was to evaluate the efficacy of the PRP injection alone, none of the patients was referred to the physical therapy unit and no pain medication was prescribed.
Results
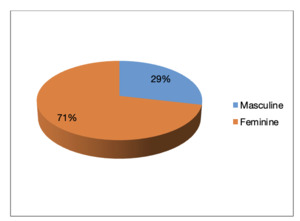
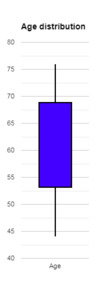
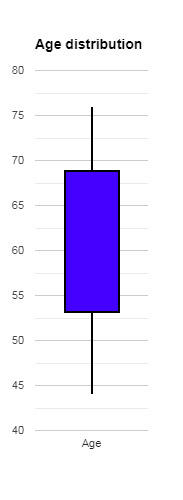
Among the 21 patients, there were 15 females (71%) and 6 males (29%) – figure 1. The mean age was 60 years, ranging from 44 to 76 years (Figure 2). All patients had grade 3 Kellgren-Lawrence KOA.
Three patients were excluded for the 4th year reevaluation because they had total knee replacements, thus allowing the authors to reevaluate 18 patients after four years of the PRP injection.
According to data on the 18 patients’ medical files, there was no other information about further invasive treatments after the PRP injection. During the follow up consultation, all 18 patients confirmed there were no other treatments besides pain killers and non-steroidal anti-inflammatory drugs.
Comparing pre- and post-PRP injection VAS scale and Lysholm questionnaire, the authors observed improvement in both scores.
Pre-injection VAS medium score was 7 (range 5 to 9, median 7). VAS improved to 2 (range 0 to 5, median 1) after one week, 4 weeks (range 0 to 8, median 2) and 8 weeks (range 0 to 7, median 2). In the 4-year reevaluation, the medium VAS was 4, ranging from 3 to 5 with a median value of 4. Figure 3 illustrates the VAS before and after the injection.
In figure 4, the distribution of pain scores according to the VAS is shown. VAS scores were higher in the pre injection evaluation. The majority of patients reported pain scores over 7. After one week, we observe a wide reduction of pain scores but with great variability among patients. This also occurred after four and eight weeks, but with some patients reporting no pain. After four years, the majority of patients reported a level 3 or 4 pain score, with less variability.
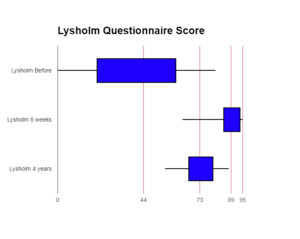
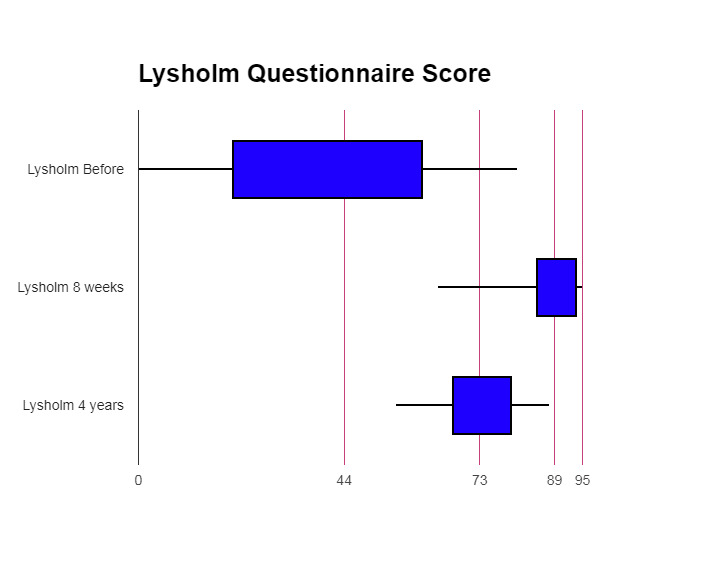
The distribution of Lysholm questionnaire scores can be observed in figure 5. Lysholm questionnaire had more variability in the pre injection evaluation with lower scores. At 8 weeks and at 4 years, this distribution changed to a narrower one, but with higher scores.
Pre-injection Lysholm questionnaire medium score was 41, ranging from 9 to 73, with a median of 44. At the eighth week evaluation, there was improvement of the medium score to 84, ranging from 52 to 95 (median 88). In figure 6 we can see the status pre-injection and at eight weeks.
Despite the exclusion of three patients, the remaining 18 patients maintained the improvement in Lysholm scores after four years, although there was some degradation of these results. The medium score after four years was 73, ranging from 50 to 85 (median 73) (Figure 7).
About the excluded three patients, they had initial VAS scores of 7, 9 and 7, which initially improved to 5, 6 and 2 at the first week but after 8 weeks the pain score hadn't improved significantly, staying at 5, 7 and 3. These three patients had low scores in the pre-injection Lysholm questionnaire (26, 9, 51) and at the 8-week reevaluation these scores were 52, 87 and 95.
Discussion
Osteoarthritis is the most common form of degenerative joint pathology and is a major cause of pain and functional disability (Attia et al. 2021). There are a number of publications in the literature demonstrating the therapeutic and regenerative benefits of platelet-rich plasma (PRP) injections as a treatment for knee osteoarthritis (KOA).
In the present study, the author compared pre- and post-PRP injection VAS and Lysholm scores in a series of 21 patients that were available to reevaluate after one, four and eight weeks after the injection.
For the purpose of this study, the authors applied the Portuguese language validated version of Lysholm questionnaire. Peccin et al in 2006 concluded that this translation and cultural adaptation was proven to be reproducible and valid in patients with meniscal injury, anterior cruciate ligament injury, chondromalacia and knee arthrosis (Peccin, Ciconelli, and Cohen 2006).
The authors observed an important improvement both in VAS and Lysholm scores at eight weeks. After four years from the injection, 18 patients were reevaluated and our results demonstrated a long term maintenance of this improvement in both scores, although there was slight reduction in absolute values.
Since none of the 18 reevaluated patients in our work received any form of invasive treatments during the four years period between consultations and were followed up by their general practitioner, we think there is low risk of interference in the four year outcome of the PRP injection in this group of patients.
These results are similar to the findings of Ahmad et al (Ahmad et al. 2018) and Jevsevar et al (Jevsevar 2013). These authors noted that at the 6-months (Ahmad et al. 2018) and 1-year (Jevsevar 2013) reevaluation after PRP injection there was functional improvement and pain relief, according to the International Knee Documentation Committee (IKDC) and VAS scores.
As in our study, Küffer and Ziltener corroborate that intra-articular injections of PRP allow a significant analgesic effect and functional improvement (Küffer et al. 2022).
In a systematic review containing 739 patients, Meheux et al (Meheux et al. 2016) reported significant improvements in clinical outcomes including pain and physical function post-injection, with an average follow-up of 38 weeks. This was also observed in our series of patients, who had pain and functional scores still better than the initial pre-injection scores after four years.
Moretti et al (Moretti et al. 2022) highlighted that PRP injections represent a useful conservative treatment to reduce pain, improve quality of life and functional scores at the midterm of six months follow-up in patients with knee osteoarthritis. They observed the reduction of pain was obtained already one month after injection with the best results observed after six months. In the present paper, the author observed the same results, but in a shorter time and which lasted for more than this six months period.
We observed similar results as Guillibert et al (Guillibert et al. 2019). These authors performed a single PRP injection (in their study 8.8mL ± 1.1mL) which provided significant clinical benefit to more than 80% of patients at three months, in stage 2 or 3 Kellgren–Lawrence KOA. In our study, in including only Kellgren-Lawrence grade 3 KOA, PRP injection contained 6mL of pure PRP, which gave similar results to Guillibert et al (Guillibert et al. 2019).
Patel et al (Patel et al. 2013) evaluated 78 patients (156 knees) with bilateral KOA. They observed there was no statistically significant difference between a single injection and two injections in their work, implying equal benefit of treatment in both.
Rastogi et al (Rastogi et al. 2016) on the other hand recommended that the volume for knee-specific injection should be 9 mL. In our work we used the Zimmer-Biomet PRP kit that was designed to proportionate 6mL of pure PRP in one injection. For this reason, a further study will be designed to compare the effects of 6mL PRP injection to 9mL.
Halpern et al noted clinical and VAS improvement with only one PRP injection (Halpern et al. 2013). In their work, they used a 6mL PRP injection and evaluated 15 patients at six months and one year after the injection. All patients were evaluated by the VAS and WOMAC (Western Ontario and McMaster Universities Arthritis Index) scales. Their results were similar to our observation after four years from the injection.
During the preparation of this manuscript, we observed a few papers reporting long-term results after a single PRP injection. We reevaluated 18 from 21 patients after four years from the injection. Our results showed improvement in pain and functional scores in the long-term, even though with a slight increase in pain in comparison to the short-term results.
This study has some weaknesses in which the sample size was small and there was no control group.
We conclude that in our group of patients with Kellgren-Lawrence grade 3 knee osteoarthritis a single injection of 6mL PRP could provide improvement in pain and functional status that lasted for four years. Further studies are recommended to compare the 6mL injection to the 9mL injection and with a bigger sample size. The use of a standardized PRP preparation kit that respects high quality preparation rules and gives high quality of pure PRP to be injected is a mandatory necessity.